System: Cardiovascular: Heart: Inflammatory: Rheumatic Mitral Stenosis

System: Cardiovascular: Heart: Inflammatory: Rheumatic Mitral Stenosis


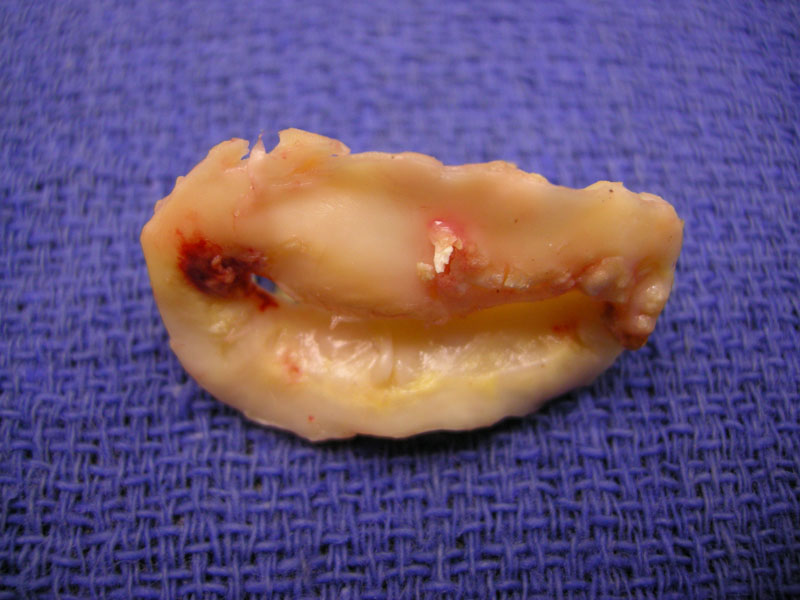
This excised mitral valve is viewed from the left ventricular aspect. The valve shows a "fish mouth" stenosis due to severe commissural fusion. There are also some areas of calcification.
The leaflets are markedly fibrotic. There is chordal fusion and shortening.
The calcifications are seen here, as they involve the opening.
The proximal chordae show intervening fibrosis and capillary proliferation consistent with old sarc. Aschoff nodules are rarely encountered in such surgical specimens. Image
In acute rheumatic valvulitis, the mitral valve is affected in the majority of cases (75%), with simultaneous mitral and aortic involvement in an additional 20%. Small verrucous vegetations are found along the lines of closure, which are composed histologicaly of fibrin and mononuclear cells. Aschoff nodules may arise in the valves or the myocardium, which consist central fibrinoid necrosis and inflammatory cells. Healing lesions show granulation tissue. A pancarditis is often found.
Acute rheumatic heart disease is a sequelae of an altered immune response to Group A beta-hemolytic streptococcus. There is T-cell cell-mediated stimulation which is thought to result in cardiac injury in the susceptible host. Clinical signs of acute infection occur 2-6 weeks after initial pharygitis.
A diagnosis of acute rheumatic fever is diagnosed in those with serologic evidence of preceding infection plus either (1) 2 major Jones criteria (carditis, polyarthritis, chorea, erythema marginatus, subcutaneous nodules) or (2) one major plus 2 minor Jones criteria (fever, elevated ESR, positive C-reactive protein, or prolonged P-R interval on EKG). The frequency of cardiac involvement in infected individuals varies from 50-70%
In post-rheumatic mitral valve disease, only about half the patients recollect a history of acute rheumatic fever. An interval as long as 10-20 years may exist between the acute rheumatic fever and the clinical development of chronic valvular disease.
The condition affects women more commonly than men. Symptoms often develop in the 3-4th decade, although may appear in adolescents in the underdeveloped nations. Symptoms initially experience dyspnea on exertion followed by orthopnea and left-sided heart failure as the condition progresses. Patients are at increased risk for infective endocarditis and thrmoboembolic events.
Mechanical treatment including surgery or percutaneous valvuloplasty is indicated for patients with pulmonary venous congestion. Valvulectomy involves an attempt to retain the posterior leaflet, but severe chordal thickening may preclude its salvage.
Cardiovascular Pathology, MPP book series 40, 2nd edition. Ed by Virginia LiVolsi. W.B. Saunders. 2001.