System: Lower Respiratory : Lung: Reactive: Diffuse Alveolar Damage

System: Lower Respiratory : Lung: Reactive: Diffuse Alveolar Damage


Organizing phase is demonstrated here with expansion of alveolar walls by fibroblasts.
Young fibroplasia (loose myxoid fibroblastic tissue) and reactive type II pneumocytes are seen here in the organizing/proliferative phase.
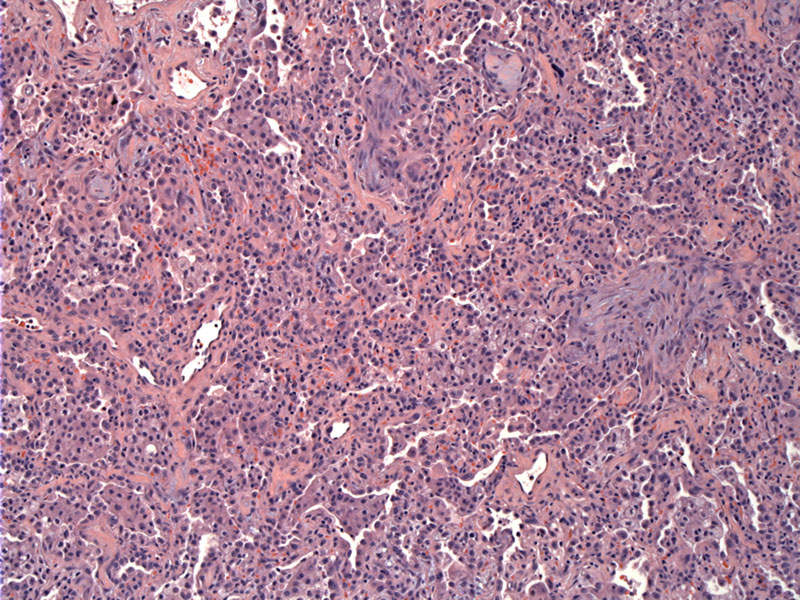
Fibrosis and increased cellularity can be appreciated in the organizing phase. Hyaline membranes (a feature of the acute phase) are not prominent in this phase as the membranes are either ingested by macrophages or incorporated into the alveolar interstitium.
Yet another image of fibrosis and intraalveolar foamy cells (which contain ingested debris).
Diffuse alveolar damage is often associated with acute respiratory distress syndrome (ARDS), and the terms are often interchangably used. In fact, diffuse alveolar damage is the most common histologic pattern seen in ARDS.
DAD is usually divided into an acute (exudative) and organizing (proliferative) phase (Kumar, Zander).
In the acute phase (days 1-5), the lungs are heavy, red and consolidated due to congestion, edema (interstitial and intra-alveolar), inflammation and fibrin deposition. Characteristic hyaline membranes (composed of cellular debris and plasma proteins) line the alveolar walls -- these membranes are very similar to those seen in hyaline membrane disease of neonates. Inflammation is usually absent or sparse.
The organizing phase begins at day 5-7, and the lungs more fibrotic with a firmer yellowish cut surface. Type II pneumocytes proliferate to repair the damaged alveolar walls. The hyaline membranes are phagocytosed by macrophages or becomes incorporated into interstitum of "repaired" alveolar walls. This repair involves proliferation of interstitial cells and deposition of collagen, with the end result being intra-alveolar fibrosis and thickening of the alveolar septae.
ARDS is characterized by a rapid onset of respiratory insufficiency, leading to severe hypoxemia and mechanically ventilation is usually required. ARDS usually develops within 24-48 hours of the inciting event, which can include sepsis, viral and bacterial pulmonary infections, gastric aspirations, mechanical trauma such as head injuries, inhaled irritants, hypersensitivity reactions -- the list goes on. Chest X-rays show diffuse alveolar involvement.
Includes steroids and supportive measures. Mortality can be as high as 60%. Those who survive regain normal pulmonary function in a year, however, some degree of pulmonary fibrosis may be present (Zander).
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 715.
Zander DS, Farver CF. Pulmonary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2008: 155-9.