System: Gastrointestinal: Liver: Autoimmune: Primary Biliary Cirrhosis

System: Gastrointestinal: Liver: Autoimmune: Primary Biliary Cirrhosis


Case 1: This 50 year old woman was AMA-positive (1:160). The bile duct is surrounded by inflammatory cells and in fact, intraepithelial lymphocytes are quite evident.
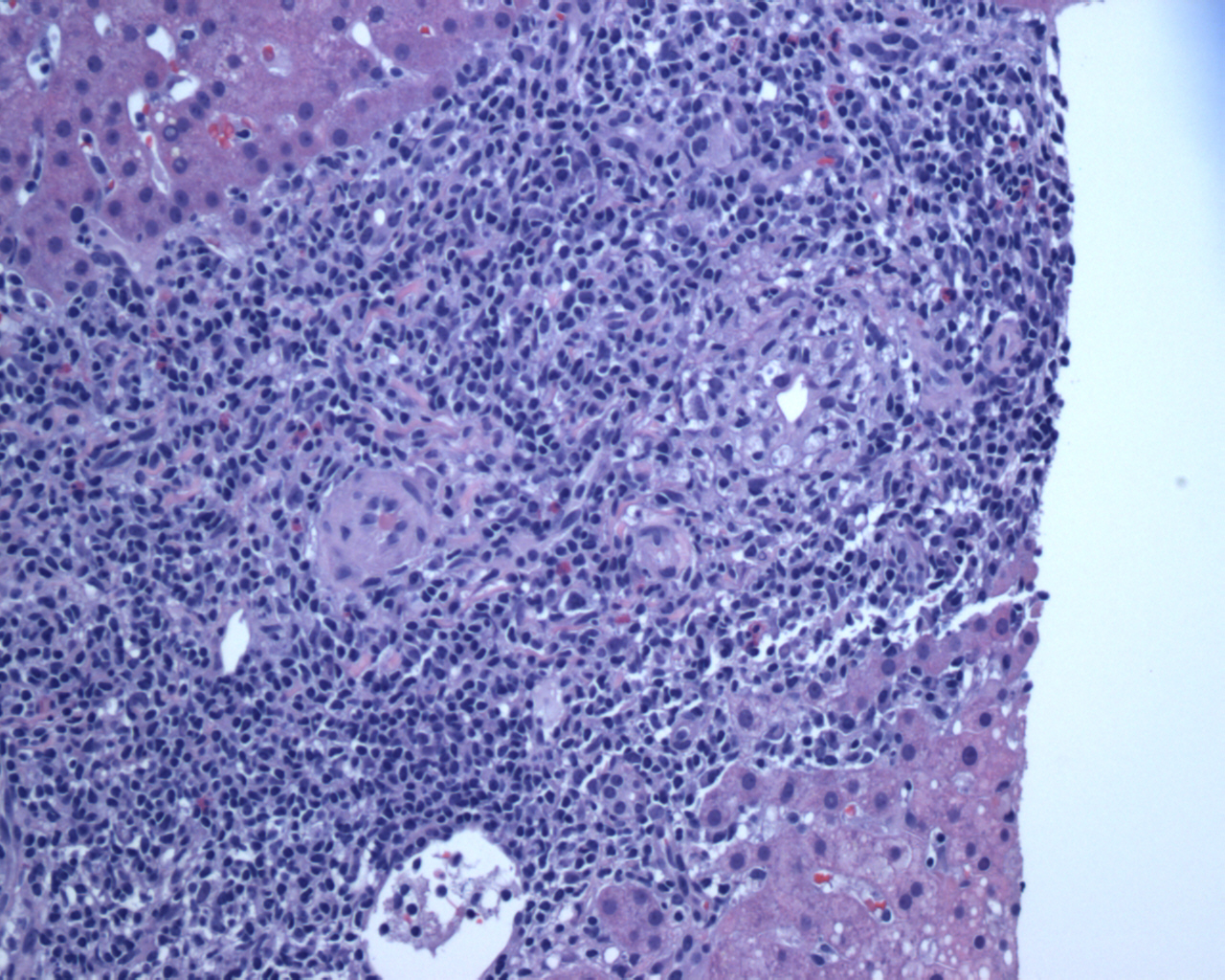
An example of granulomatous inflammation in the bile duct i.e. florid duct lesion. Remember that all you need for a granuloma are a collection of epithelioid histiocytes.
At higher power, the epithelioid histocytes can be seen more closely, surrounding the duct. The granulomas in PBC are non-caseating.
Another example of granulomatous inflammation in the portal area.
A PAS stain can not only highlight the PAS globules in alpha-1-antitrypsin deficiency, but also the basement membranes of ductules. This is helpful when the ductal architecture is obscured.
Case 2: Portal tract expansion is due to a ductular proliferation and fibrosis. A mild lymphocytic infiltrate is also seen. Granulomas adjacent to damaged bile ducts (not seen here) can be extremely helpful when present.
There is a proliferation of abnormal ductules with curvilinear shapes and closed lumens in a fibrotic stroma.
Intraductal cholestasis due to obstruction of bile flow, seen as brown concretions within the bile ducts. Bile plugs are also seen in the hepatic lobules.
Primary biliary cirrhosis (PBC) is characterized by destruction and loss of small interlobular bile ducts. PBC is seen predominantly in women in their 50s to 70s and is associated with other autoimmune disorders such as Sjogren disease (dryness of eyes and mouth), thyroiditis, rheumatoid arthritis and celiac disease
In the early stages, one finds the classic florid duct lesion, which consists of a dense inflammatory infiltrate in the portal tracts and injury to the bile duct epithelial cells. Granulomatous destruction of the bile ducts is especially helpful in supporting the diagnosis, but well-formed granulomas may not always be found. The inflammatory infiltrate consists of lymphocytes, some eosinophils, macrophages and plasma cells. Intraepithelial lymphocytes are commonly identified within the bile ducts (Iacobuzio).
The gross and histologic features of PBC depends on the chronicity of the disease, and the name may be misleading since cirrhosis does not occur until the very late stages of the disease process.
As the the disease progresses, there is bile ductular proliferation, fibrosis, piecemeal necrosis and chronic cholestasis. In late stage PSC, there may be loss of bile ducts with prominent cirrhosis. Grossly, the liver is bile stained with micronodular cirrhosis (Kumar, Iacobuzio).
PBC should be distiguished from primary sclerosing cholangitis (PSC). The latter is more likely to affect males, demonstrate periductal fibrosis -- and florid duct lesions with granulomatous inflammation is not a feature of PSC.
90% of PBC affects women with peak age of diagnosis between the 5th and 7th decade. Presents with fatigue, pruritis (due to accumulation of bile salts). Lab findings linclude elevation of serum alkaline phosphatase and cholesterol. Antimitochondrial antibodies are present in 90-95% of patients (Kumar).
Ursodeoxycholic acide (a synthetic bile acid) has been employed, although overall survival benefits remain controversial. Liver transplantation is an option for those with end stage liver disease (Kumar, Iacobuzio).
Prognosis relates to the disease stage at the time of diagnosis. Asymptomatic patients survive around 15 years, whereas those who present with symptoms live a median of only 7.5 years. There is an increased risk of developing hepatocellular carcinoma.
→The histopathology of PBC varies depending on the stage of disease ranging from the classic florid duct lesion in early stages to micronodular cirrhosis in late stages.
→Presents with fatigue and pruritis. Patient may have other autoimmune diseases (ie. Sjogrens).
→Lab findings include elevated alkaline phosphatase and presence of antimitochondrial antibodies (AMA-positive).
• Liver : Chronic Hepatitis C Grading (Activity)
Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005:563-8.
Kumar V, Abbas AK, Fausto N et al. Robbins and Cotran Pathologic Basis of Diseases. 8th Ed. Philadelphia, PA: Elsevier; 2010: 867-8.
Scheuer PJ, Lefkowitch JH. Liver Biopsy Interpretation 7th Ed. Philadelphia, PA: Elsevier; 2006: 69-79.