
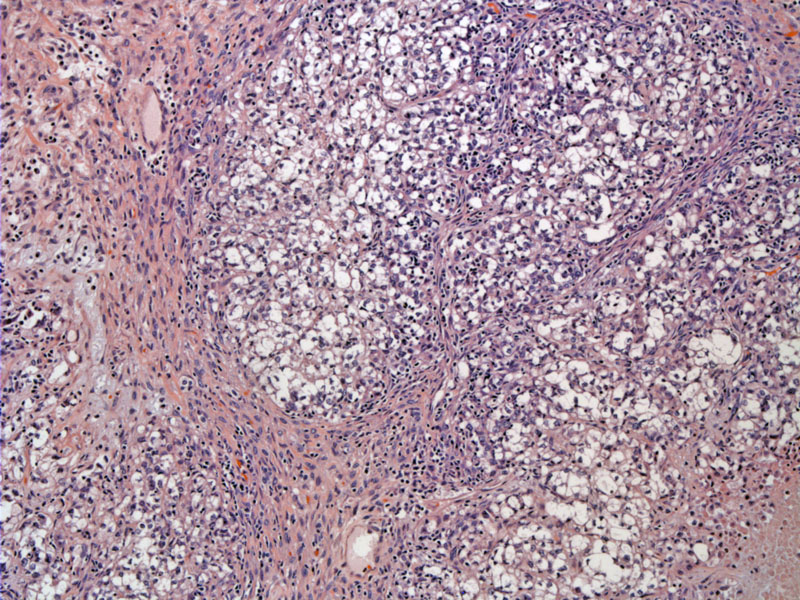
Clear cell carcinomas show a variety of patterns, with irregular vague lobular areas of solid growth illustrated here.
In tubulocystic areas, the clear cells line the walls of the cystic spaces and often appear as single cells in the lumen.
The cells are polyhedral with clear cytoplasm; the nuclei are often eccentric placed -- pushed aside due to abundant cytoplasm.
Tumor necrosis is common in clear cell carcinoma, as seen in the lower left field. In this area, the cells have are closely pack with limited cytoplasm, features which are not necessarily seen extensively in this tumor.
Cytological exam of intraoperative pelvic washings shows cohesive groups of extremely large overlapping malignant cells with prominent nucleoli. Compare their size with the benign cells in the background.
The corresponding cell block exhibits malignant cells with eosinophilic and focally clear cytoplasm.
A different patient with clear cell carcinoma of the ovary presented with ascites. The cellular material reveals markedly enlarged cohesive clear cells on the cell block preparation.
Glandular structures are also present, lined by these same pleomorphic clear cells.
The monolayer shows cells which are easily several times as large as the background lymphocytes and mesothelial cells. The hobnail pattern is still visible in this preparation.
Cohesive tumor cell clusters are three-dimensional on the monolayer.
Yet another case demonstrates the common tubulocystic pattern.
Other areas reveal back-to-back glands and broad papillae growing into dilated spaces. Note the presence of pink amorphous hyalinized material, some of which are round and line the inside of glandular lumens. These hyaline bodies are usually found in the stroma and within cells.
A solid focus with blue mucinous material within glandular lumina is seen.
Papillae are lined by pleomorphic clear cells. Some cells bud off and appear free floating.
Clusters of papillae imparts an almost solid look. The papillary cores are mildly hyalinized in this image. Prominent hyalinization of papillary cores is often a helpful diagnostic feature as this is usually not seen in other surface epithelial carcinomas.
The edge of a larger cystic space is shown with a sclerotic stromal background. Variably sized cystic glands are seen.
Clear cell carcinoma of the ovary arise from surface epithelium or from foci of endometriosis. Although benign and borderline cases do exist, the overwhelming majority (over 90%) of clear cell neoplasms of the ovaries are carcinomas that exhibit aggressive behavior. There is a uniquely strong association with hypercalcemia and endometriosis.
Grossly, these tumors tend to be large and range from 10-30 cm in diameter. They are usually solid with cystic areas. Approximately 30% are bilateral. Microscopically, three cell types are found: (1) clear cells: polygonal or cuboidal cells with abundant optically clear cytoplasm containing glycogen. The nuclei are centrally or eccentrically located and may be vesicular with prominent nucleoli; (2) cells with eosinophilic cytoplasm: similar to clear cells in size, shape and nuclear features, however, the cytoplasm is granular and eosinophilic; (3) hobnail cells: the cytoplasm can be either clear or eosinophilic. The trademark feature is hyperchromatic nuclei that protrude into lumens like hobnails.1
The cells may be arranged in a variety of patterns such as glandular, tubular, tubulocystic, papillary or solid. Sometimes, eosinophilic hyaline globules may be found in the stroma or scattered within the neoplastic cells.
Most often occurs in post-menopausal women (6th to 7th decades). Two-thirds of women are nulliparous. Presents with enlarging abdominal mass, and thus is often detected in a clinically advanced stage. Other common findings include hypercalcemia. Interestingly, women with clear cell carcinoma are more likely to present with thromboembolic events (DVT and pulmonary emboli).
A significant portion of clear cell carcinomas are associated with ovarian or pelvic endometriosis. These tumors can arise within endometriosis and also, as a mixed tumor with endometrioid carcinoma. Supporting evidence includes the following: 50-70% of clear cell carcinomas are associated with pelvic endometriosis; 25% of clear cell carcinomas arise within an endometriotic cyst; 20-25% of clear cell carcinomas are mixed with endometrioid carcinoma.2
Treatment is as for epithelial ovarian cancers. This consists of complete surgical staging and tumor debulking with a total hysterectomy, bilateral salpingo-oophorectomy, pelvic lymphadenectomy, omentectomy, washings, and peritoneal biopsies of the pelvis, abdomen, and diaphragm. Optimal debulking consists of leaving no residual disease greater than 1 cm. Surgery is following with a platinum and taxane based chemotherapy regimen, Recurrences are treated with a diverse range of chemotherapy regimens, with platinum remaining the mainstay of therapy.
Clear cell carcinomas are virtually all high grade, and they have a worse outcome (stage for stage) compared to other epithelial ovarian tumors. The grading of these tumors in the ovary does not appear to have prognostic value. 5 year survival for stage I and stage III disease is ~70% and ~30% respectively.2
♥ There is a strong association with endometriosis. Up to 70% are associated with endometriosis, 25% arise within an endoemetrioic cyst and 25% are mixed with an endometrioid carcinoma component.
♥ Hypercalcemia is a frequent finding.
♥ Histologic grading has not shown to be predictive as virtually all are high grade and aggressive tumors.
• Endometrium : Arias-Stella Reaction
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 584-5.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 432-436.
3 Mills SE, ed. Sternberg's Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2562-8.