
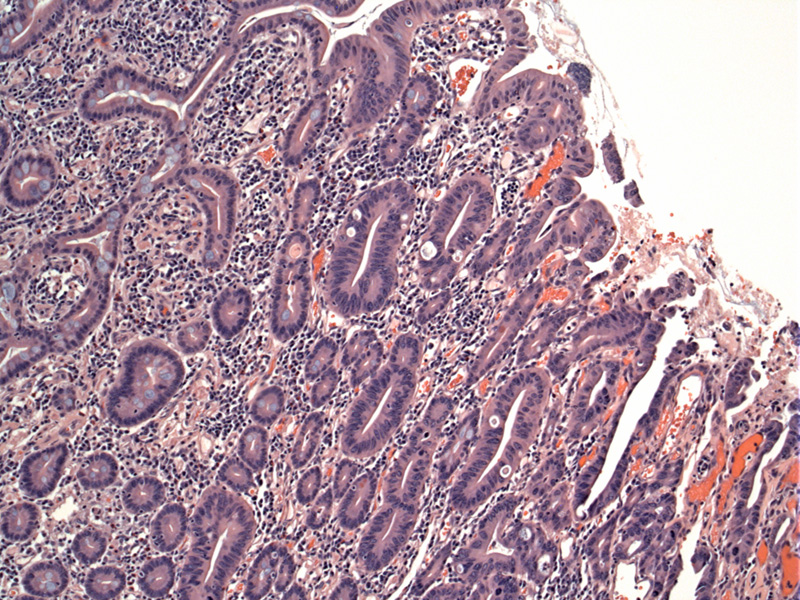
While most small bowel adenocarcinomas are found in the duodenum, this unusual one arose from the jejunum. Normal enteric mucosa is seen in upper left, with adenomatous changes occurring in the right part of the image.
More carcinoma in situ (high grade dysplasia) changes can be appreciated here within the surface mucosa.
Invasion through the muscularis propria is extremely common. About 2/3 of tumors stain for keratin 7 and keratin 20, which may help differentiate them from colorectal adenocarcinomas in which less than 5% show this pattern.
The tumor shows extensive involvement of subseroal fat, consistent with T3 and is typical of small intestinal malignancies.
While the small bowel occupies 90% of the surface area and 75% of the length of the alimentary tract, neoplasms of the small bowel is very rare. Benign neoplasms such as adenomas and mesenchymal tumors are more common while malignant neoplasms are indeed exceptional, accounting for only 1% of all GI malignancies or approximately 1000 deaths in the US (Kumar). The most common malignant neoplasms in the small intestine are adenocarcinomas, followed by carcinoid tumors, lymphomas and sarcomas.
Adenocarcinomas of the small intestine display the same adenoma-dysplasia-carcinoma sequence seen in the colon. Most cases arise sporadically, however, certain conditions place an individual at increased risk for developing these neoplasms including polyposis syndromes (FAP, HNPCC, Peutz-Jegher, juvenile polyposis), Crohn disease and celiac sprue. Patients with FAP have a 100-200 fold risk for developing adenocarcinoma of the small intestine, and those with Crohn disease or celiac sprue have an 80 fold risk (Iacobuzio).
The large majority of adenomas and adenocarcinomas occur in the duodenum, where 65% arise in the periampullary region. The exception to this proximal (duodenal) location is Crohn disease where the primary site of inflammation and hence carcinogenesis is the ileum.
Grossly, tumors in the duodenum and periampullary region arise as exophytic masses, whereas as more distal lesions in the jejunm and ileum tend to be annular (napkin-ring) and constricting. Histologically, these neoplasms are similar to their colorectal counterparts with complex glands and luminal necrosis. In contrast to colorectal adenocarcinoma where invasion into the lamina propria is considered carcinoma-in-situ or Tis due to the lack of lymphatics in the colorectum, invasion into the lamina propria is considered stage T1 as the small bowel is flush with intramucosal lymphatics (Iacobuzio).
CK7/CK20 IHC studies will be helpful in distinguishing small intestinal adenocarcinoma (CK7+/CK20+) from metastatic colorectal adenocarcinoma (CK7-/CK20+).
Presents in older adults with average age of diagnosis at age 67 (Iacobuzio). Symptoms (in order of frequency) may include: nausea/vomiting, abdominal pain, melena, weight loss, anemia, palpable abdominal mass, dyspepsia, intestinal obstruction, and jaundice (Chaiyasate).
Surgical resection. There are few clinical studies on the role of chemotherapy (primarily 5-FU) but it does not appear to have a significant impact.
Small bowel adenocarcinomas are regarded as highly fatal. By the time of diagnosis, these neoplasms are usually at an advanced stage with invasion into the bowel wall or other adjacent structures. Metastasis to liver and regional lymph nodes arev common. Furthermore, small intestinal adenocarcinomas lack responsiveness to chemotherapy. 5-year survival rates range from 20% to 30% (Chaiyasate, Dabaja), although en bloc wide excision has yield a 70% 5 year survival rate in some cases (Kumar).
In one large review, a statistatical difference in survival was found for histological grade: median survival 66 months for well-differentiated tumors; 40 months with moderately differentiated tumors and 14 months with poorly differentiation (Chaiyasate). Nodal negative patients also survival longer (78 months), whereas, nodal positive patients showed a median survival of 26 months. Tumor stage is also highly significant.
Small intestinal adenocarcinomas usually present with high stage and have a very poor prognosis.
The majority involve the duodenum (especially the ampulla), although patients with Crohn disease develop them in the ileum.
Co-expression of keratin 7/20 helps exclude metastatic disease from the colorectum.
• Small Intestines : Adenocarcinoma with Mucinous Features
Chaiyasate K, et al. Prognostic factors in primary adenocarcinoma of the small intestine: 13-year single institution experience. World J Surg Oncol. 2008 Jan 31;6:12.
Dabaja BS, et al. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer. 2004 Aug 1;101(3):518-26.
Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 174-8.
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 857.
Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 729-730.