System: Bone: Osseous: Neoplastic: Conventional Osteosarcoma, High Grade

System: Bone: Osseous: Neoplastic: Conventional Osteosarcoma, High Grade


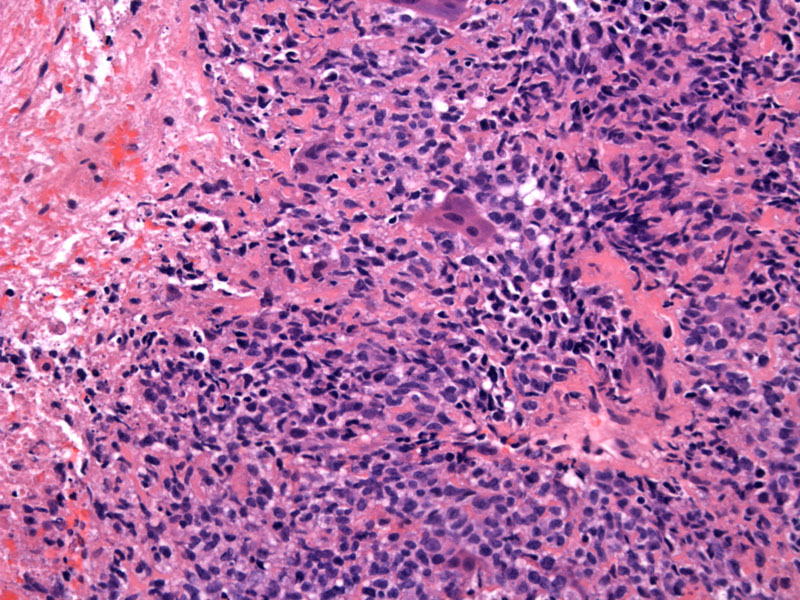
High grade conventional osteosarcoma demonstrating pleomorphic tumors cells making non-mineralizing osteoid.
Up to 50-60% of the tumor demonstrate spontaneous necrosis.2
The tumor is high grade as shown by its extreme celluarity of tumor cells, numerous atypical mitotic figures, and necrosis, the latter seen in the prior image.
A highly cellular stroma contains scattered osteoclast giant cells as well.
The gross appearance of osteosarcomas can be fleshy, cystic, bony or hemorrhagic depending on proportions of bone, cartilage, stroma and vessels.4 . In this image, the tumor demonstrates an admixed fleshy and hemorrhage cut surface, and the cortex has been replaced entirely by tumor growth.
Another osteosarcoma with an admixture of stroma (white-tan and fleshy), hemorrhagic and cartilaginous (gelatinous) component showing obviously aggressive growth.
This distal femur is involved by an osseous mass with cortical disruption to evolve into a large soft tissue mass.
a different case - shows broad zones of malignant osteoid Image
cells intercolating within osteoid and giant cell Image
necrotic osteoid Image
necrosis in upper left Image
Corresponding film for the resection specimen Image
another angle, same patient Image
Osteosarcomas, the most common primary malignant bone tumor, mesenchymal tumors in which the neoplastic cells produce bone matrix (Kumar). There are numerous variants of osteosarcomas, but the underlying key feature is the direct production of osteoid by tumor cells, without intervening cartilege.
Approximately 75% of osteosarcomas are of the conventional type, and 25% are variants with significant differences in morphology, clinical setting and prognosis.1 There are many different ways osteosarcomas and its variants are subclassified, and we shall briefly describe a simple scheme in Fletcher's Diagnostic Histopathology of Tumors.3
Fletcher initially partitions the tumors into two broad categories by location of the tumor: within the bone (the majority) and on the surface of the bone (a minority). These categories are then further subdivided by clinical, histologic and radiographic features.
Osteosarcoma within the bone: |
| Conventional osteosarcoma (osteoblastic, chondroblastic, fibroblastic) |
| Small cell osteosarcoma |
| Telangeictatic osteosarcoma |
| Low-grade central osteosarcma |
| Osteosarcoma in Paget disease |
| Postradiation osteosarcoma |
| Osteosarcoma in other benign processes |
Surface osteosarcomas: |
| Parosteal osteosarcoma |
| Periosteal osteosarcoma |
| High-grade surface osteosarcoma |
Osteosarcomas exhibit a bimodal distribution. 75% of cases affecting patients younger than 20, and the second smaller peak occurs in the elderly with predisposing conditions such as Paget's disease and a history of prior radiation.
Conventional osteosarcomas mostly occur between age 10-25, and are located in the metaphysis of the long bones (at the site of greatest bone growth) with 60% the distal femur or proximal tibia. Presents with pain, swelling and sometimes, pathologic fracture.
Depending on the nature of the matrix produced by the tumor cells, conventional osteosarcomas can be osteoblastic (50%), chondroblastic (25%) and fibroblastic (25%). These histologic variants have no prognostic importance, however.3 Metastasis to the lung is common as ~10-20% demonstrate pulmonary mets at the time of diagnosis.2
Limb-salvage surgery or amputation and chemotherapy depending on stage.
5-year survival of 60 to 70% with chemotherapy and surgery.
• Fibrous : Fibro-osseous Pseudotumor of Digits
• Fibrous : Myositis Ossificans
http://emedicine.medscape.com/article/394057-overview
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 1294-6.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1615-8.