
Proliferative fasciitis, a variant of nodular fasciitis, consists of fibroblasts in a loosely textured stroma. The proliferating cells extend along fibrous septae that compartmentalize the fat into the underlying fascia.
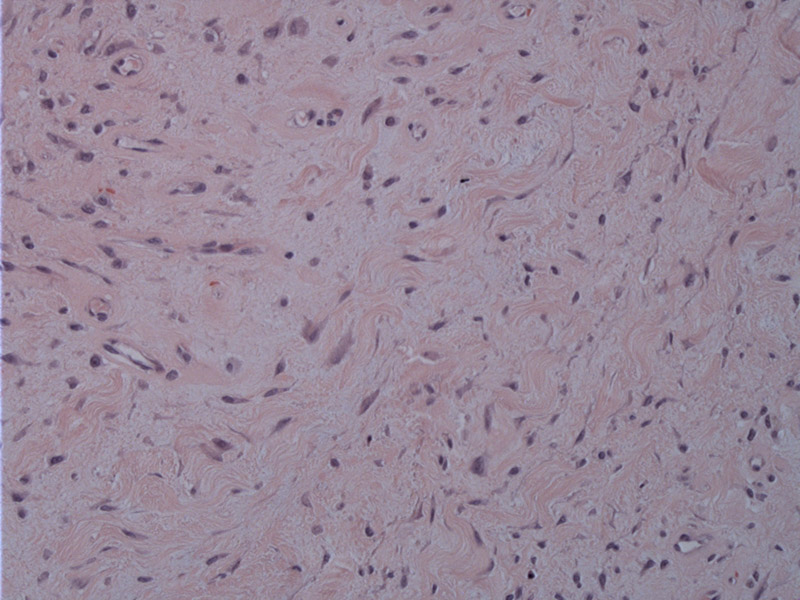
This lesion consists of proliferating cells, including spindle and stellate fibroblasts and larger, more polygonal cells that morphologically mimic ganglion cells.
The hallmark of this lesion are these ganglion-like cells that have abundant basophilic cytoplasm, 1 or 2 nuclei, and large, prominent nucleoli. Some appear
Proliferative fasciitis, similar to nodular fasciitis, grows rapidly and is self-limited and benign in nature. However, it affects an older population. The peak incidence of proliferative fasciitis is in the 6th decade versus the 4th decade for nodular fasciitis. Furthermore, proliferative fasciitis occurs in both the upper and lower extremities, whereas nodular fasciitis is concentrated in the upper extremity, especially the forearm.
Grossly, the lesion is somewhat less circumscribed that nodular fasciitis. The spindled proliferation mainly involves the interlobular fibrous tissue septae of the subcutis (Wu) and range 1 to 7 cm in size.
Histologically, the key distinguishing feature is the presence of ganglion-like cells scattered among the fibroblasts. These polygonal or rounded cells have darkly staining cytoplasm and vesicular nuclei with prominent nucleoli.
These ganglion-like cells also bear some resemblence to rhabdomyoblasts, and in children, proliferative fasciitis can consist largely of thse ganglion-like cells, and thus, elicit concern for rhabdomyosarcoma at first glance (Folpe, Fletcher). However, IHC stains implicates a myofibroblastic lineage (Rosai).
Benign reactive process. Similar to that of nodular fasciitis.
→ A variant of nodular fasciitis, the key feature is the presence of ganglion-like cells
• Fibrous : Ischemic fasciitis
• Fibrous : Proliferative Myositis
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1540-1.
Folpe AL, Inwards CY. Bone and Soft Tissue Pathology: Foundations in Diagnostic Pathology Philadelphia, PA: Elsevier; 2010: 43-5.
Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 2246.
Wu JM, Montgomery E. Classification and Pathology. Surg Clin N Am 88 (2008) 483-520.