System: Lower Respiratory : Lung: Neoplastic: Lymphomatoid Granulomatosis

System: Lower Respiratory : Lung: Neoplastic: Lymphomatoid Granulomatosis


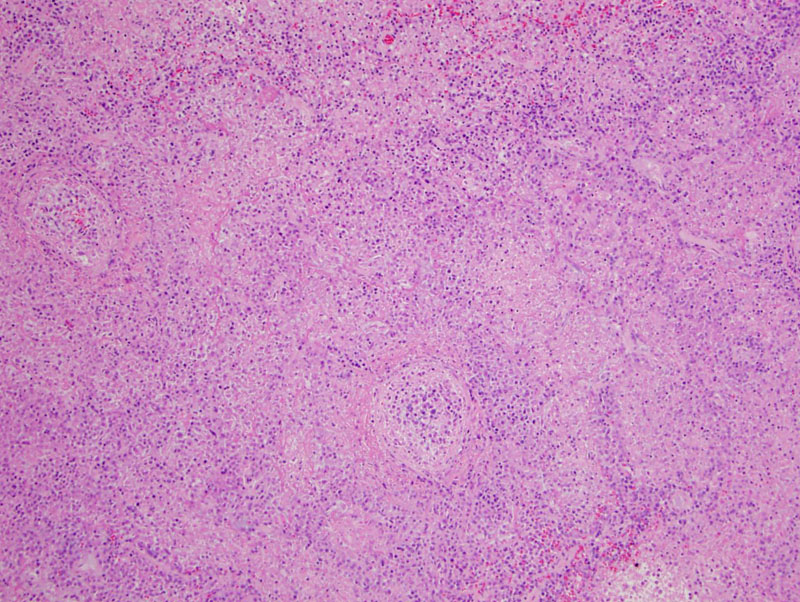
The lung parenchyma is significantly altered by an extensively necrotic lymphoid infiltrate effacing the architecture. Widespread infarction is typical.
One of the classic features of LG is angiocentric lymphocytic invasion. A closer image of a vessel demonstrates intramural lymphocytes.
Another medium-sized vessel is affected, as seen here.
There is remarkable consolidation of the lung by an atypical appearing lymphoreticular infiltrate. Image
The lymphoreticular infiltrate consists of enlarged atypical lymphocytes, small lymphocytes, histiocytes and plasma cells within the alveolar walls and encircling vessels.
LG involving small vessels of the brain is seen here. Lesions in the CNS predicts a poor prognosis.
Lymphomatoid granulomatosis (LG) is usually an EBV associated clonal B-cell proliferation with a reactive T-cell background (Fletcher). The lesion consists of enlarged atypical B-cells that often center around vessels. The nodular proliferations frequently have necrotic centers. These infiltrates consist of atypical lymphocytes as well as small lymphocytes and histiocytes.
LG typically involves the lungs but may also affect other organs such as the CNS, skin, and kidneys. Pulmonary nodules composed of lymphoid and plasmacytoid cells are characteristic, and occasionally these infiltrates invade vessels and mimic vasculitis, especially Wegener's Granulomatosis. One-half of patients eventually develop a lymphoid malignancy, most commonly non-Hodgkin lymphoma (Kumar).
LG is graded 1-3 depending on the number of EBV infected cells demonstrated on in-situ hybridization. Grade I lesions contain rare (less than 5/hpf) EBV-positive cells; grade II lesions contain 5-20/hpf; and grade III lesions contain greater than 20/hpf. Note that grade III lesions meet the criteria for malignant lymphoma (Zander).
Affects both adults and children of all ages, with median age at diagnosis is 60 (Zander, Flethcer). There is a 2:1 male to female ratio. Patients present with cough, dyspnea, and chest pain. Extrapulmonary disease such as skin rashes (30%), CNS lesions (30%), kidney (30%) can occur. LG often occurs in the setting of immunocomprising conditions such as HIV, post-transplanation (though renamed post-transplant lymphoproliferative disorder) and defective cell-mediated immunity (Fletcher).
Treatment includes chemotherapy, interferon a2b and anti-CD20 antibiodies (Zander).
Spontaneous remission occurs in 14-27% of patients, and up to 67% die from the disease. Poor prognostic factors include higher grade lesions, older age and CNS involvement (Fletcher, Zander).
LG is EBV associated and affects immunocompromised individuals.
The histologic triad of LG: (1) atypical B-cell proliferation, often with mixed small lymphocytes and histiocytes; (2) angiocentric invasion; and (3) coagulative necrosis.
• Lung : Wegener Granulomatosis
Cheng L, Bostwick DG, eds. Essentials of Anatomic Pathology. 2nd Ed. Totowa, NJ: Humana Press; 2006: 956.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1205-6.
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 542.
Zander DS, Farver CF. Pulmonary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2008: 474-6.