
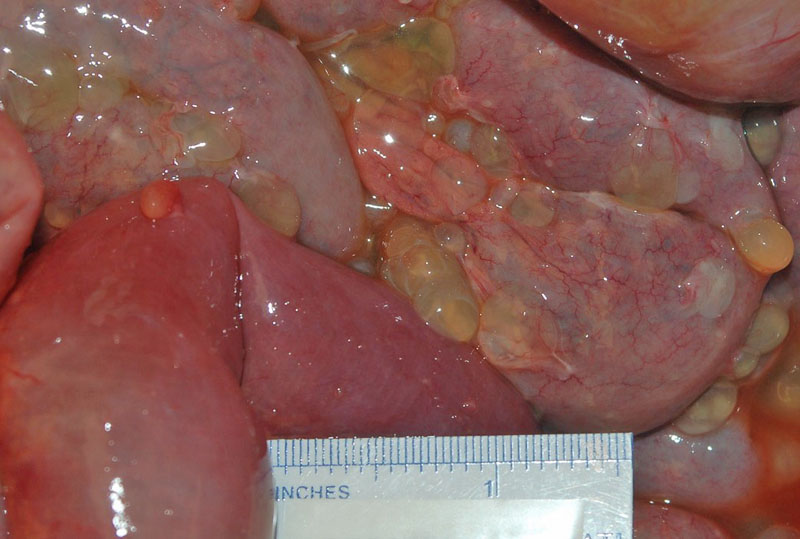
The bowel is diffusely studded with small thin walled cysts filled with clear to tan fluid arranged in grapelike clusters.
Multiple fluid-filled, thin-walled translucent cysts are collected. The intracystic fluid varies from clear to blood-tinged and may occasionally be mucinous or gelatinous. They are actually quite pretty in a disturbing sort of way.
Microscopically, the cysts are multilocular and lined by a single layer of flat or cuboidal mesothelial cells; cysts are separated by fibrous septa, which often reveal acute and chronic inflammation, and mild cytological atypia may be seen.
Areas of pink fibrin (lower half of image) are a common feature.
A proliferation of entrapped granulation tissue in the cyst wall is also a common finding.
Benign multicystic peritoneal mesothelioma (BMPM) is also known as multilocular peritoneal inclusion cysts (MPIC), inflammatory cysts of the peritoneum and post-operative peritoneal cysts. It is a rare lesion arising from the abdomino-pelvic cavity, mostly in reproductive-age women. Cases in children, postmenopausal women and men have been reported. About 150 cases have been described in the literature (Baratti).
Some authors believe because of BMPM's association with inflammatory processes (e.g. prior surgery, endometriosis and pelvic inflammatory disease), it may be a reactive process with mesothelial cell proliferation and secondary cystic changes rather than a true clonal neoplasm.
This neoplasm is most frequently encountered in women of reproductive age. The average age at diagnosis is approximately 32 years (Amesse). Pelvic/abdominal pain is the most common presenting symptom.
There is a strong association with previous abdominal surgery, endometriosis and pelvic inflammatory disease (Safioleas). There is no reported association with asbestos exposure (Baratti).
Complete surgical resection is recommended; successful treatment with tamoxifen has been reported in single cases, resulting in a reduction of the cyst volume and growth.
Although benign, recurrence after surgical treatment has been reported in about half of the patients (Fletcher). Other than incomplete resection at initial surgery, neither the size and localization or pathological features are valuable predictors for recurrent disease.
• Peritoneum : Peritoneal inclusion cyst
Amesse LS, Gibbs P, Hardy J et al. Peritoneal inclusion cysts in adolescent females: a clinicopathological characterization of four cases. J Pediatr Adolesc Gynecol. 2009 Feb;22(1):41-8.
Baratti D, Vaira M, Kusamura S, et al. Multicystic peritoneal mesothelioma: outcomes and patho-biological features in a multi-institutional series treated by cytoreductive surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Eur J Surg Oncol. 2010 Nov;36(11):1047-53. Epub 2010 Sep 15.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 882-4.
Safioleas MC, Constantinos K, Michael S, et al. Benign multicystic peritoneal mesothelioma: a case report and review of the literature. World J Gastroenterol. 2006 Sep 21;12(35):5739-42.