System: Skin: Melanocytic: Neoplastic: Blue Nevus

System: Skin: Melanocytic: Neoplastic: Blue Nevus


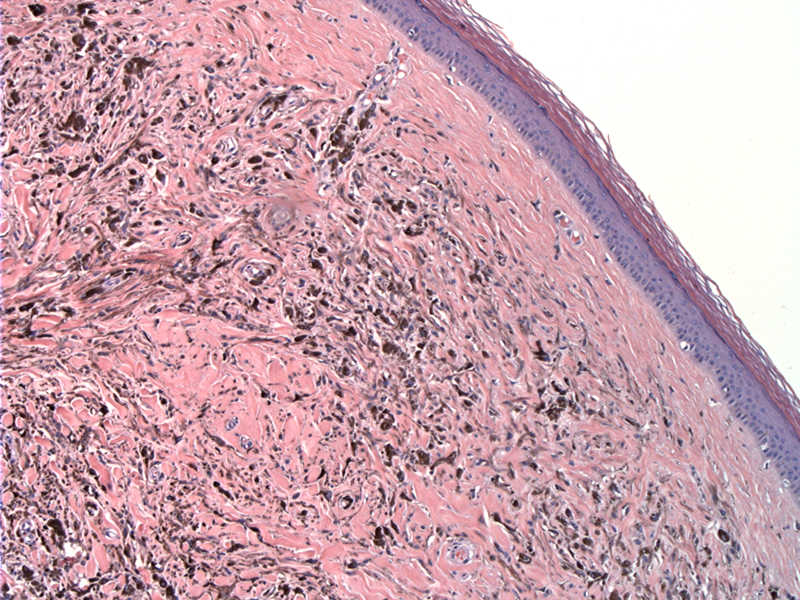
Common blue nevi are well-circumscribed, pigmented, dermal spindle cell lesions with a normal overlying epidermis. There is no junctional component. The pigment is located predominately within dermal melanophages which may dominate the dermis making the dermal melanocytes inconspicuous within the prominent stroma. The lesional melanocytes are found often around adnexal structures or neurovascular bundles.
Blue nevi can be wedge-shaped with the base of the wedge parallel to the epidermis and the pigmented cells lying parallel to the epidermis.
Dermal dendritic melanocytes are the lesional cell with elongated cytoplasmic processes, giving them a spindle-cell shape. The dendritic melanocytes are variably pigmented with small hyperchromatic nuclei and they lack mitotic activity and atypia. These dendritic melanocytes are intermixed with intermediate and neurotized melanocytes and prominent melanophages that contain melanin granules giving them a heavily pigmented appearance.
A collagenous, prominent stromal response is typical among dermal melanocytes and melanophages.
Although there are many clinical and pathologic variants, two variants of blue nevus are most commonly discussed, the common blue nevus and the cellular blue nevus. They are relatively common lesion resulting from arrested melanocytic migration in the dermis when melanocytes are traveling from the neural crest. Their name is due to the blue hue imparted to the skin because of the depth of the melanin pigment.
All variants of blue nevus share the following features: blue appearance, dermal spindle cell proliferation among melanin pigment within melanophages and melanocyte lesion cells, sclerotic stroma and focal HMB-45 staining.
Multiple blue nevi may be associated with 1. LAMB syndrome, which is represented by lentigenes, atrial myxoma, mucocutaneous myxoma and blue nevi and 2. nodular mastocytosis. Blue nevi can mimic metastatic melanoma when satellite nodules are present.
Deep penetrating blue nevus may be confused with melanoma, as a result if the nevus's variation of nuclear size and shape. Other variants of blue nevi include combined, sclerosing/desmoplastic, hypomelanocytic/amelanotic , pigmented epithelioid melanocytoma and malignant blue nevi.
Common blue nevi occur as a single nodule less than 1.0 cm in size that have a predilection for the dorsal hands and feet, scalp and buttocks, although rarely they are found other places (ie. uterus, prostate, cervix). They are typically acquired lesions of adulthood with a 2:1 female predominance (but can occur congenitally or at any age).
Cellular blue nevi are nodules/plaques measuring greater than 1.5 cm, which is larger than common blue nevi. They are usually found on the lower back or buttocks in adults less than 40 years. Cellular blue nevi are usually painless unless they degerate or ulcerate.
Simple excision is sufficient.
Blue nevi are nearly always benign and rarely, they may recur after excision.
→Blue nevi are dermal dendritic melanocyte proliferations that appear blue on clinical exam and have prominent melanophages among a prominent collagenous stroma.
→It is important to recognize blue nevi as it can mimic malignant melanoma histologically.
1 Sternberg SS, ed. Diagnostic Surgical Pathology. 5th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009: 85-86.
2 Murali R, McCarthy SW, Scolyer RA. Blue nevi and related lesions: a review highlighting atypical and newly described variants, distinguishing features and diagnostic pitfalls. Adv Anat Pathol. 2009 Nov;16(6):365-82.
3 Artur Zembowicz, Pushkar A. Phadke. Blue Nevi and Variants: An Update. Arch Pathol Lab Med. 2011; 135:327-36.
Author: Nichole Steidler MD, Dept of Pathology at University of New Mexico