
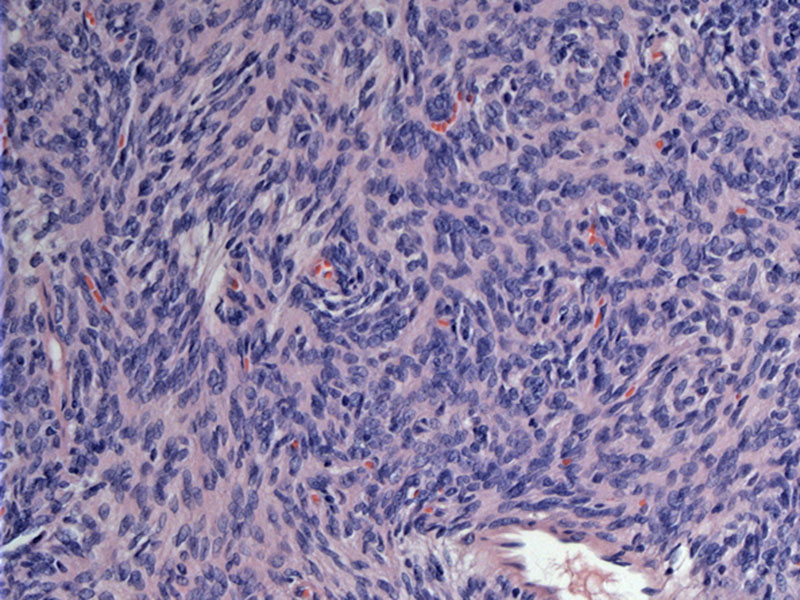
Case 1 - This case shows the characteristic features of type A thymoma. Epithelial cells are spindled in shape and arranged in a fascicular or storiform pattern. There are a few scattered lymphocytes.
The spindled cells have dense chromatin and indistinct nucleoli. The cytologic features should be bland. Some dense fibrosis is seen as well.
Case 2 - The tumor contains more epithelioid cells with some microcystic alteration.
Pseudorosettes are also seen in a small percentage of type A thymomas. These structures are seen devoid of a lumen. The epithelial cells in this type can range from spindled to more oval and cuboidal.
Cysts of various sizes may also a feature, with some larger ones as well. The cells lining these larger cyst become attenuated. Some cysts may become macroscopic and contain proteinaceous material or histiocytes.
Yet another image of larger cysts and hemangiopericytoma-like vessels. True glandular lumens containing secretions may be encountered in some tumors, but are not seen here.
Thymoma can manifest a variety of morphological appearance, and one must keep in mind that the subclassification of thymoma has been a subject of debate for many years and remains one.
WHO type A thymoma is characterized by a neoplastic population of oval to spindle cells lacking marked cytological atypia, admixed in variable proportions with small (usually few) lymphocytes. This type of thymoma is synonymous with the “spindle‐cell or medullary thymoma” in the traditional classifications. This type is rather uncommon (<10%) among thymomas (Davis, Fletcher). Features seen in type A include pseudorosettes without a true luemn, glandular formations (often subjacent to the tumor capsule) and cystic spaces (Rosai, Fletcher).
Thymoma classification is confusing. Here's how I keep it straight. Type A thymomas are composed of spindled or sometimes oval epithelial cells without atypia. Type B thymomas are composed of more rounded, plump "epithelioid" spindle cells with more cytoplasm. Type B thymomas are separated into B1, B2 and B3, with the difference being the proportion of lymphocytes. Type B1 is comprised largely of lymphocytes and just scattered epithelial cells whereas type B3 is mostly epithelial cells with very few lymphocytes. Type B2 lies somewhere in between. Type C thymoma (thymic carcinoma) can also spindled in morphology with few lymphocytes (like type A), but there is marked cytologic atypia.
Complete surgical resection is the treatment of choice.
Prognosis is excellent with type A thymoma. Recurrence is highly unlikely with this subtype, as is disease related death. 5 to 10 year survival is nearly 100%. Most cases (91-94%) of type A and AB thymomas have stage I or II disease. In contrast, as you move from B1 to B3 thymomas, the stage is more advanced (stage III or IV)(Fletcher).
Type A thymoma is characterized by bland spindled to ovoid epithelial cells and few intraepithelial lymphocytes, if at all
Many architectural patterns exist, including solid sheets, rosettes, glands, and hemangiopericytoma-like patterns
Type A best corresponds to the medullary thymoma of the MH system
Davis WD, Brambilla E et al. Tumours of the Lungs, Pleura, Thymus and Heart: The WHO Classification of Tumours. 1st Ed. IARC, Lyons; 2004.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1323-1327.
Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 477.