System: Mediastinum: Thymus: Developmental: Severe Combined Immunodeficiency

System: Mediastinum: Thymus: Developmental: Severe Combined Immunodeficiency


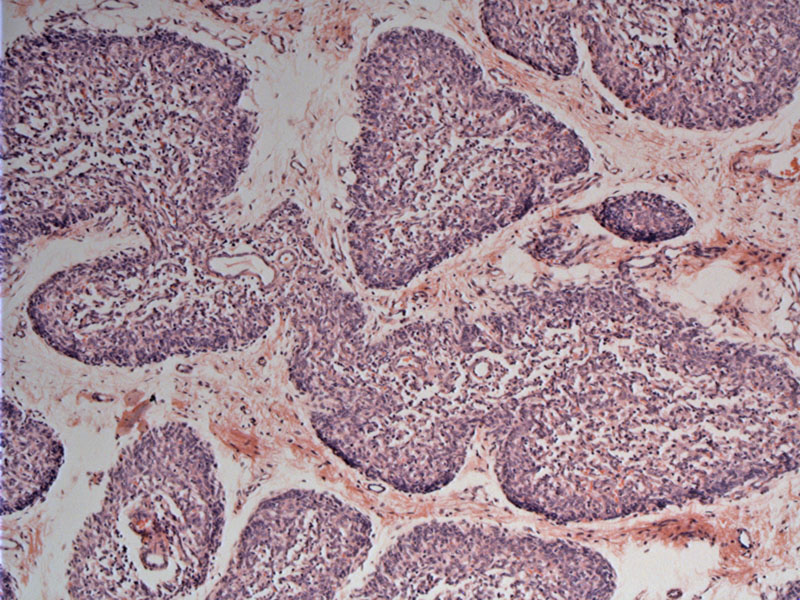
discrete medullary islands Image
Thymic cortex is extremely reduced and consists of densely packed thymic epithelial cells. Image
depletion of lymphoid cells is obvious, but note also the lack of differentiation of the thymic epithelium, responsible for the absence of Hassal's corpuscles Image
The incidence is estimated to be 1 per 100,000 live births, and affected infants rarely live beyond their first birthday without treatment. Although infants with SCID appear to have one disease, more than 15 separate single-gene defects have been described (smart. The result is an arrest in T-cell development, which causes a profound decrease in T lymphocytes.
About one half of cases are X-linked, and one half are autosomal recessive. Infants with this primary immunodeficiency disorder are at risk for graft-versus-host disease because they lack the ability to reject foreign tissue, such as maternal T cells that cross into the fetal circulation in utero.
Severe skin rash with red, peeling skin resembling eczema often develops in the first few weeks of life. Skin superinfection with S. aureus occurs frequently (Smart). Recurrent, severe, and sometimes fatal infections occur with common viruses such as adenovirus, parainfluenza, and varicella. Recurrent mucocutaneal and esophageal infections with Candida can may occur and result in failure to thrive (Smart). Bacterial infections including otitis media, pneumonia, and skin infections are seen frequently. Opportunistic infections (PCP, CMV) are the hallmark of a T-cell immune defect, conditions which should prompt investigation for this disease.
Infants manifest profound T-cell lymphopenia, with less than 20% T cells, as compared with 55% to 75% for normal infants. B-cell numbers may be low, normal, or increased.
Bone marrow or stem cell transplantation performed within the first 3 months of life offers a 95% survival rate (Myers; Buckley). Prior to transplantation, prophylaxis against PCP pneumonia with trimethoprim-sulfamethoxazole, intravenous gammaglobulin, avoidance of all live vaccines, and the use of CMV-negative, leukodepleted, irradiated blood products is indicated.
The natural outcome is poor and most die by the age of 1 year. For those undering bone marrow transplantation, there remains a frequent deficiency of B cells. Even for those whose B cells do engraft, the majority are unable to produce normal amounts of immunoglobulins and have to be treated long-term with immunoglobulins.
Smart BA, Ochs HD. The molecular basis and treatment of primary immunodeficiency disorders.
Curr Opin Pediatr. 1997 Dec;9(6):570-6.
Buckley R, Schiff S, Schiff R, et al. Hematopoietic stem-cell transplantation for the treatment of severe combined immunodeficiency. N Eng J Med. 1999;340(7):508–516.
Myers LA, Patel DD, Puck JM, et al. Hematopoietic stem cell transplantation for severe combined immunodeficiency in the neonatal period leads to superior thymic output and improved survival. Blood. 2002;99:872–878.
Nezelof C. Thymic pathology in primary and secondary immunodeficiencies. Histopathology. 1992 Dec;21(6):499-511.