System: Breast: Proliferative Disease Without Atypia: Benign: Usual Epithelial Hyperplasia

System: Breast: Proliferative Disease Without Atypia: Benign: Usual Epithelial Hyperplasia


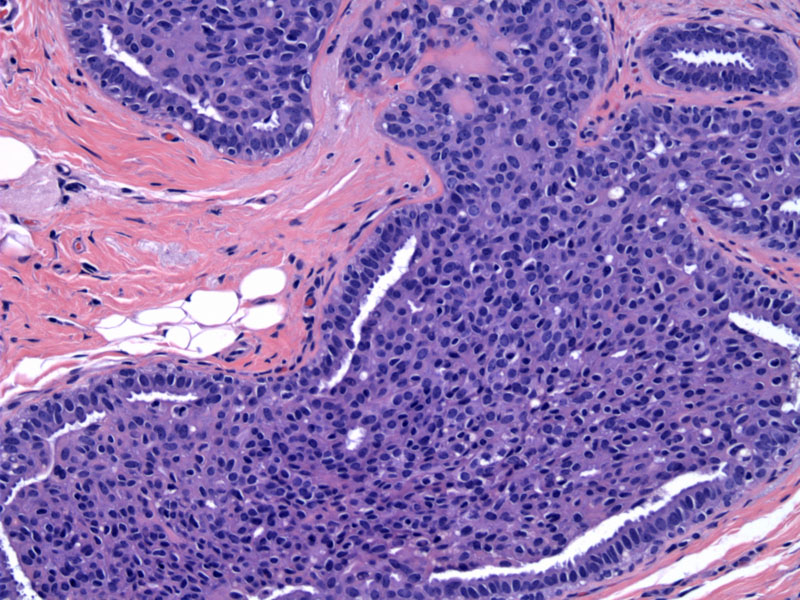
This image demonstrates the key features of florid usual epithelial hyperplasia: (1) a heterogeneous cell population composed predominately of epithelial cells and a smaller population of myoepithelial cells. There is also a smattering of lymphocytes (2) a streaming, swirling, haphazard arrangement of cells (3) slit-like luminal spaces, especially in the periphery.
moderate ? Image
mild ductal hyperplasia Image
Epithelial hyperplasia is best thought of as a spectrum changes, ranging from mild hyperplasia (conferring no added risk of breast cancer), to moderate/florid hyperplasia (small risk of breast cancer), atypical ductal or lobular hyperplasia (moderate risk) and finally LCIS or DCIS (high risk).
Mild hyperplasia is defined as no more than 4 cell layers above basement membrane. Remember that the usual structure consists of a myoepithelial and lumenal epithelial layer, so only two layers. Moderate hyperplasia is defined as five or more cell layers; bridging within the lumenal space may be present. Florid hyperplasia occurs when the entire lumen is distended with hyperplastic cells. There is no clear cutoff between moderate and florid hyperplasia, however, this doesn't matter since moderate and florid hyperplasia are placed in the same risk category.
Usual epithelial hyperplasia does not have a corresponding mammographic lesion; it is generally found in conjunction with other radiologically detectable breast lesions such as cysts and radial scars. These lesions may contain microcalcifications, therefore, microcalcifications is not a useful feature in separating usual epithelial hyperplasia from atypical hyperplasia or DCIS.
If moderate/florid hyperplasia is present, patient has minimally elevated risk and should be continued to be followed by mammography.
Patients with mild hyperplasia have no increased risk of developing breast cancer, and those with moderate/florid hyperplasia have up to a two-fold increase in risk, which may not be clinically significant. For example, a 40 year old women has a baseline risk of developing breast cancer of 1/1000 per year, and doubling this risk would result in a 2/1000 risk per year.2
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007:919-920.
2 O'Mallye FP, Pinder SE. Breast Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2006:159-164.