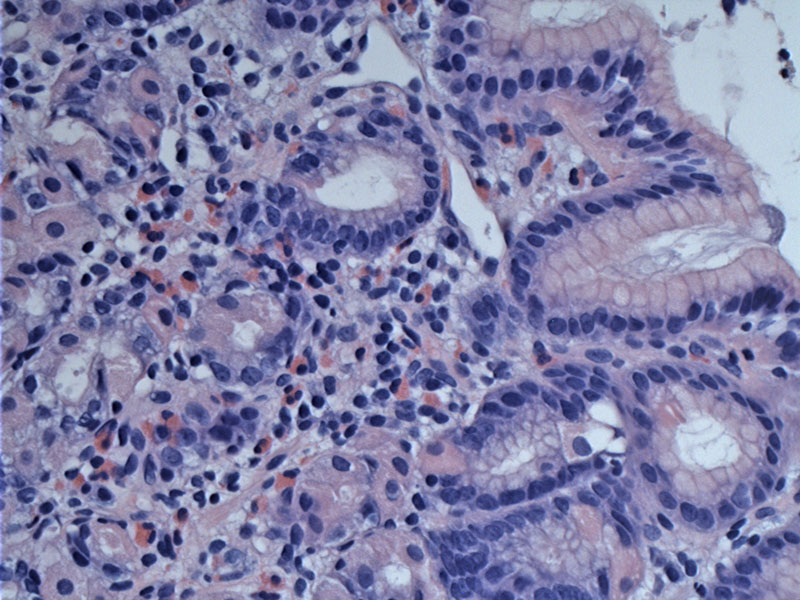
There are increased eosinophilis in the lamina propria along with some lymphocytes. This finding may be patchy -- thus small or only a few biopsies may miss the pathology due to insufficient sampling.
Eosinophils are quite numerous in this additional case.
The superficial mucosa shows edema which is quite marked.
Eosinophils are seen dispersed alongside lymphocytes and plasma cells.
Some flattening of the mucosa and erythema are appreciated.
Eosinophilic gastroenteritis (EG) is uncommon, characterized by a variably intense eosinophilic infiltration of the gastrointestinal tract. Any portion of the GI tract from the esophagus to the rectum may be involved.
It is important to remember that eosinophils normally reside in the lamina propria of the GI. The exception is the esophagus, which ought to be devoid of eosinophils in the nonpathologic state. The actual number of eosinophils necessary to trigger a diagnosis of EG is debated among experts (Khan).
When it affects the stomach, the gastric mucosa may seem normal or may show ulcers and erosions. Definitive diagnosis requires the presence of symptoms and a biopsy with increased eosinophils and usually associated epithelial damage. Nondiagnostic biopsies may be obtained due to the patchy nature of the process.
It affects all races and any age group, although in adults, it usually presents in the third to fifth decade. Eosinophilic proctocolitis is almost exclusively seen in children.
A personal or family history of food allergies and atopic disorders are found in 25% to 70% of cases (Khan). Patients may have elevated serum eosinophils (peripheral eosinophilia) or elevated levels of IgE. The most common presentation is abdominal pain, although bleeding, dysmotility, obstruction and ascites may also be seen.
Clinical manifestations vary depending on the depth of bowel wall involvement. For example, mucosal involvement leads to abdominal pain, vomiting and diarrhea. Involvement of the muscularis leads to obstructive symptoms such as gastric outlet syndrome. Serosal involvement may lead to bloating and ascites (Nyugen, Khan).
Eosinophilic gastroenteritis may also be secondary to a number of conditions including inflammatory bowel disease, autoimmune diseases, drug reactions and infections (e.g. H. pylori).
Steroid treatment usually yields an excellent response in symptoms. Some cases may result in gastric outlet obstruction, requiring surgical intervention (Holroyd).
• Esophagus : Eosinophilic Esophagitis
Holroyd, et al. Transmural eosinophilic gastritis with gastric outlet obstruction: case report and review of the literature.Ann R Coll Surg Engl. 2010 May;92(4):W18-20.
Kahn S. Eosinophilic gastroenteritis. Best Practice & Research Clinical Gastroenterology (2005); 19(2): 177-198.
Nyugen MT, Szpakowski JL. Eosinophilic gastroenteritis: eMedicine. Last updated on June 15th 2009. Available at: emedicine.medscape.com/article/174100-overview