
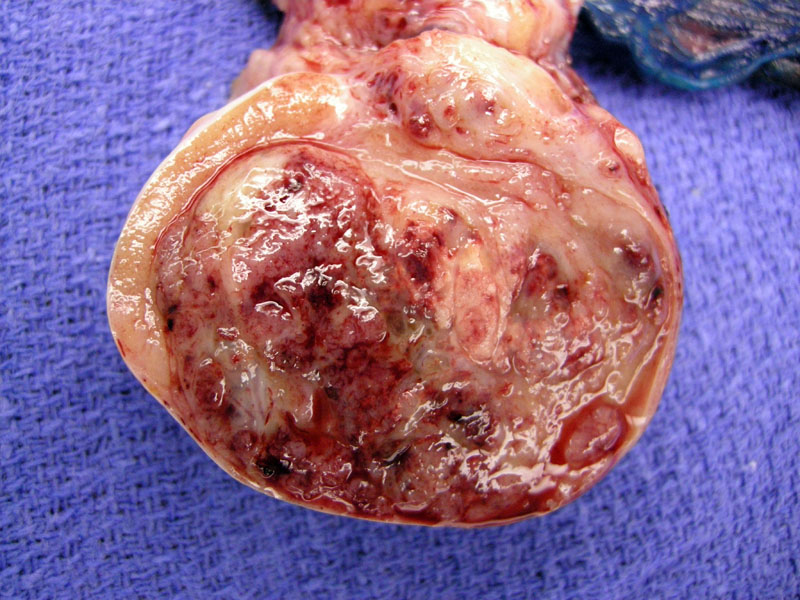
This 5 cm embryonal carcinoma demonstrates a highly variegated cut surface, with hemorrhagic areas admixed with tan zones. It appears fairly well-delineated, with a rim of normal parenchymal to the left. This tumor did show lymphovascular invasion. Overall in 20% of cases, the tumor extends through the tunica albuginea into the epididymis.1
Microscopically, the neoplastic cells form several patterns: acinar, tubular, tubulocystic, papillary, solid sheets and a peculiar aggregation called embryoid bodies. 1,2 This embryonal carcinoma demonstrates a mixture of patterns, with neoplastic cells lining broad projections of fibrous stroma.
Markedly anaplastic cells with hyperchromatic nuclei containing vesicular chromatin and prominent nucleoli. The cell borders are indistinct with overlap of nuclei, lending a disorganized syncytial look.
CD30 staining demonstrates a strong membranous pattern in embryonal carcinoma .Cytokeratins, PLAP, and OCT4 are also usually positive; AFP may be focally positive and hCG positivity is only seen in syncytiotrophoblastic giant cells.1,3
A tubular pattern is seen in this region of the tumor. The pleomorphic cells have indistinct cell borders. Areas of necrosis and hemorrhage are usually present.
Other areas show a more convincing papillary pattern. The nuclei are hyperchromatic with prominent nucleoli.
Embryoid bodies consist of a discrete central portion of embryonal carcinoma with a clear space surrounding it.
Intratubular embyronal carcinoma (seen here) and intratubular germ cell neoplastia (ITGCN) may be found in the periphery of the tumor. These are not unusual for this neoplasm.
Lymphovascular invasion is present. Rather than single tumor cells floating in this vascular lumen, there are adhesed cells along the endothelial lining, corroborating the interpretation of true invasion.
Primitive mesenchymal stroma is often associated with embryonal carcinoma. This finding by itself does not warrant an additional diagnosis of teratomatous elements.
Embryonal carcinoma is usually found as a component of a mixed germ cell tumor, however, it can be found in its pure form. When 'pure' tumors are examined as a whole, the most common type is a seminoma, followed by embryonal carcinoma.
However, this assertion depends on the exact definition of embryonal carcinoma, which differs depending on which text you read. For example, if AFP immunoreactivity in focal cells (which highlights the yolk sac component) disqualifies the tumor from being 'pure' embryonal carcinoma, the number of pure embryonal carcinoma drops dramatically. This particular entity could be signed out as an "embryonal carcinoma with yolk sac differentiation". If clear cut histologic features of yolk sac tumor were identified, then the entity would be called a mixed germ cell tumor and the pathology report would list the percentages of each subtype of tumor.1
Note that syncytial cells that stain positively for hCG or cells immunopositive for AFP may be focally present -- most pathologists do not consider these tumor a mixed germ cell tumor unless these elements make up a substantial portion of the tumor (see discussion above).2
Occurs mostly in younger men between 25-35, presenting with unilateral painless testicular enlargement. A third of patients may present with metastasis in para-aortic lymph nodes, lungs and liver. Occasionally, serum AFP and/or hCG may be increased. These tumors are more aggressive than seminomas.1,2
Orchiectomy +/- adjuvant chemotherapy.
Stage at initial presentation is very important. Embryonal carcinoma accounting for greater than 80% of the tumor is an adverse prognostic factor as well as the presence of lymphovascular invasion.1,3
• Testis : Malignant Mixed Germ Cell Tumor
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 822-4.
2 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 1043.
3 Zhou M, Magi-Galluzzi, C. Genitourinary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2006: 548-553.