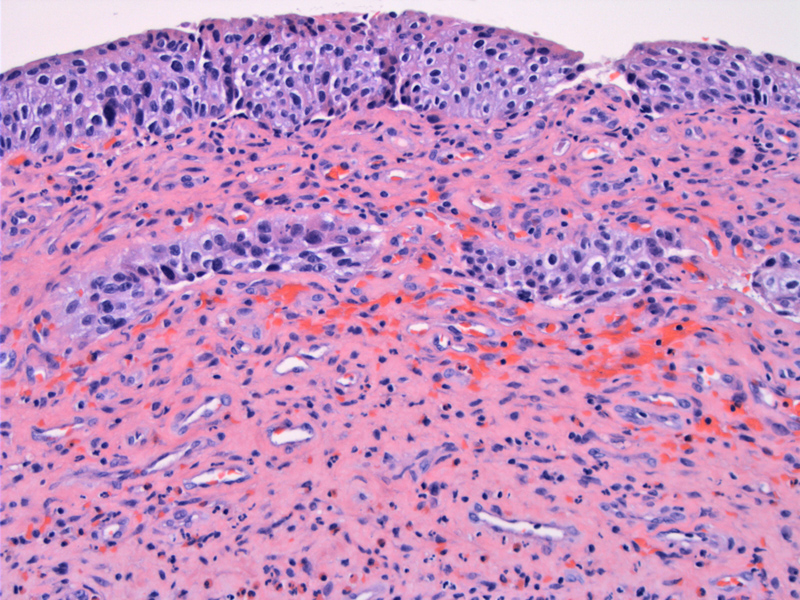
The urothelium shows some uniformly darker nuclei and some focal crowding. Not the red cells and capillary proliferatin as well.
The stroma has been altered by fibrosis of the lamina propria, replacing the muscular fibers.
There are also prominent eosinophils as well as some other chronic inflammation. A vessel shows some endothelial injury with a small area suggetive of fibrin.
The stromal cells show some slightly darkened nuclei with irregular shapes and a smudgy appearance.
Focal surface denudation and ulceration with underlying fibrin thrombi in two capillaries are seen.
Endothelial injury is evident with lifting of these cells from their basement membrane (center to slightly to the right, bottom vessel. The upper vessel shows some myointimal thickening.
The bladder is incidentally exposed to radiation in patients treated with radiation for cancer involving other pelvic organs, often the prostate.
Radiation exposure results in a diverse clinical and pathological findings. The acute and subacute phases generally occur within 3 to 6 months after therapy. Symptoms during this time may include urinary frequency, urgency and voiding pain (Marks). Gross hematuria occurs in up to 7.7% of patients and is more common in the first 6 weeks after therapy, although it has may occur as long as 14 years later (Marks;Magrine). The bladder shows urothelial desquamation, and atypia of urothelium with nuclear and cytoplasmic vacuolization. Edema, increased vascularity, and acute and chronic inflammatory cells, including eosinophils and mast cells occupy the lamina propria (Marks).
The chronic phase of radiation cystitis begins approximately 6 months after therapy, with changes attribued to ischemia due to vascular endothelial injury. The long-term sequelae are due to ischemia of the bladder wall secondary to radiation induced damage to vascular endothelial cells. One may see vascular endothelial hyperplasia, vascular occlusion and perivascular fibrosis. Normal smooth muscle is replaced by fibroblasts resulting in decreased bladder compliance and capacity. Reduced healing capacity may lead to mucosal ulceration, hemorrhage, occasional spontaneous perforation and fistula formation. Atypical stromal cells with bizarre appearing hyperchromatic smudged nuclei are often present (Chan)
Treatment is essentially symptomatic, mainly consisting of controlling the haematuria by bladder lavage. Other treatments most frequently used are intravesical instillations of formalin, silver nitrate or alum with an efficacy on symptoms of about 70% (Rigaud). Another treatment option is hyperbaric oxygen therapy, which allows better tissue diffusion of oxygen, improving neo-angiogenesis by increasing the vascular density of irradiated tissues. This technique is effective in about 80% to 90% of cases with a lasting effect (Chong; Corman).
For severe debilitating chronic radiation symptoms, hyperbaric oxygen and argon bean coagulation have been employed, but the results are highly variable.
Acute and subacute phase symptoms are generally self-limiting. More severe cases require treatment, as noted above.
• Bladder : Hemorrhagic Cystitis
• Bladder : Urothelial Carcinoma in Situ
Marks LB, Carroll PR and Dugan TC et al. The response of the urinary bladder, urethra, and ureter to radiation and chemotherapy, Int J Radiat Oncol Biol Phys 31 (1995), p. 1257.
Magrina JF. Urologic complications of radiation therapy for gynecologic malignancies, Int Urogynecol J Pelvic Floor Dysfunct 4 (1993), p. 111.
Chan TY and Epstein JI. Radiation or chemotherapy cystitis with “pseudocarcinomatous” features, Am J Surg Pathol 28 (2004), p. 909.
Rigaud J, Hetet JF, Bouchot O. Management of radiation cystitis Prog Urol. 2004 Sep;14(4):568-72.
Corman JM, McClure D, Pritchett R, Kozlowski P, Hampson NB. Treatment of radiation induced hemorrhagic cystitis with hyperbaric oxygen. J Urol. 2003 Jun;169(6):2200-2.
Chong KT, Hampson NB, Corman JM. Early hyperbaric oxygen therapy improves outcome for radiation-induced hemorrhagic cystitis. Urology. 2005 Apr;65(4):649-53.