System: Skin: Melanocytic: Malignant: Melanoma

System: Skin: Melanocytic: Malignant: Melanoma


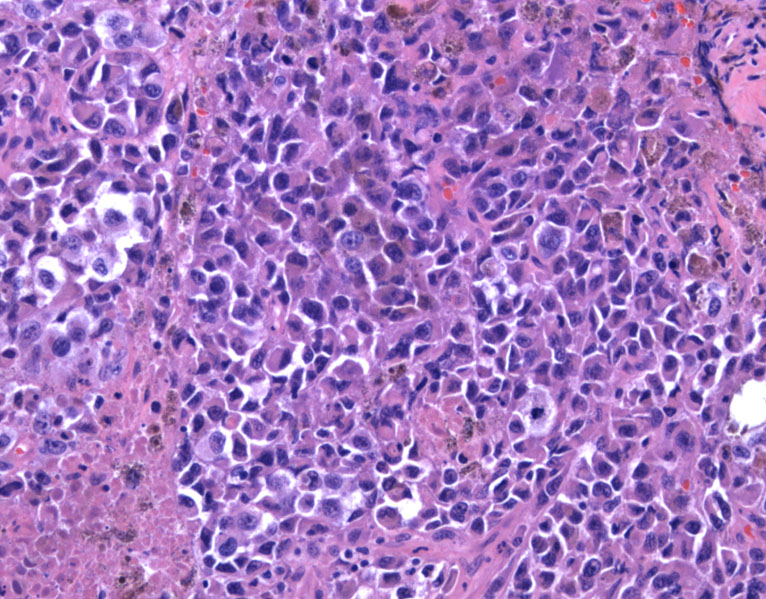
Case 1: Epithelioid malignant melanocytes are singly dispersed and infiltrating through the dermis.
Their discohesive nature is obvious.
The malignant melanocytes have eccentric nuclei, prominent nucleoli, and occasional cytoplasmic pigmentation, in a somewhat nested architecture.
The melanoma cocktail strongly positive.
Case 2: This desmoplastic variant melanoma is spindled and hypocelluar.
Case 3: This different case shows more pleomorphism and pigmentation. There are scattered lymphocytes.
Case 4: This case demonstrates pagetoid spread in the epidermis. It is extremely helpful when an in situ (intraepidermal) melanoma is present.
The deeper portion of the same lesion shows invasive nests of atypical melanocytes.
S100 highlights the numerous melanocytes in the epidermis
Case 5: The superficial spreading type is composed of well-formed junctional nests (theques) and pagetoid spread.
A high power view of reveals epithelioid atypical melanocytes in the dermis.
Case 6: Melanoma is capable of extreme degrees of nuclear atypia.
Case 7: However, spindle cell variants can have notoriously bland cytology.
The incidence of melanoma has increased dramatically in the past 20 years. In the US, it is the fifth most common cancer in women and sixth for men. In contrast to SqCC and BCC which is due to chronic sun-exposure and generally arises in sun-exposed skin, melanoma is largely due to intermittent intense sun-exposure in childhood (in fair-skinned individuals), and tends to arise in sun-covered areas. Only 1/3 arise from pre-existing nevi; 2/3 arise de novo(Rapini).
The gold standard for diagnosis is a combination of clinical history and histology, however, melanomas are famous for being tricky to diagnosis. Clinically obvious melanoma may appear benign or reactive histologically, and vice versa. Amelanotic melanoma may also add to the confusion.
There are many variants of melanoma, each with specific histologic features. The most common or conventional variants are: superficial spreading type, lentigo maligna type, nodular type and acral type. Less common variants include spindle cell, desmoplastic, neutrotropic, nevoid, Spizoid, blue nevus-like, macrophage-rich, small cell, signet rignt, balloon cell, myxoid and so on.
The histological diagnosis of melanoma does not depend on any one specific feature, but a constellation of findings. Common features in melanoma include asymmetry, ill-defined borders, large size (usually greater than 4mm, but smaller melanomas do exist), pagetoid spread or letinginous junctional proliferation of single melanocytes or nests, complex and oddly shaped junctional nests, confluence of nests or melanocytes at the dermal-epidermal junction, cytologic atypia of melanocytes, discohesion of melanocytes, mitosis, lack of maturation of melanocytes, and so on (Busam).
The most important features with diagnostic significance (7th ed AJCC) are tumor thickness (Breslow depth as measured from the granular layer to the deepest point of invasion, T1≤1.00mm, T2=1.01-2.00mm, T3=2.01-4.00mm, T4>4.00mm), tumor ulceration and mitotis (T1a=without ulceration and mitosis <1/mm2, T1b=with ulceration or mitoses ≥1/mm2). Clark level is no longer used as a staging criterion. Elevated LDH is also an important prognostic indicator, and an elevated serum LDH with *any* site of metastases places the patient at M1c (Balch).
Other features worth mentioning include lymphovascular invasion, nerve involvement (not necessarily a defining feature of melanoma and can be seen in congenital, neurotized, or blue nevi), satellites (staged as N2), tumor infiltrating lymphocytes (a favorable feature)(Busam).
Worrisome features include the ABCDE rule (asymmetry, border irregulariy, color variegation, diameter greater than 6mm and evoluation in appearance or symptoms).
Risk factors include a family history, numerous nevi, fair-skin, history of excessive sun exposure, prior history of melanoma, inherited genetic defects (e.g. xeroderma pigmentosum or familial atypical mole syndrome), and immunosuppression.
• Melanocytic : Melanoma, Superficial Spreading Type
• Melanocytic : Melanoma, Acral Lentiginous
• Melanocytic : Melanoma, Nodular Type
• Melanocytic : Melanoma, Balloon Cell Type
Balch CM, et al. Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol. 2009 Dec 20;27(36):6199-206. Epub 2009 Nov 16.
Busam KJ. Dermatopathology: Foundations in Diagnostic Pathology 1st Ed. Philadelphia, PA: Elsevier; 2010: 465-482.
Rapini RP. Practical Dermatopathology. Philadelphia, PA: Elsevier; 2005: 273-9.