System: Gastrointestinal: Pancreas: Neoplastic: Mucinous Cystic Neoplasm with Moderate to High Grade Dypsplasia

System: Gastrointestinal: Pancreas: Neoplastic: Mucinous Cystic Neoplasm with Moderate to High Grade Dypsplasia


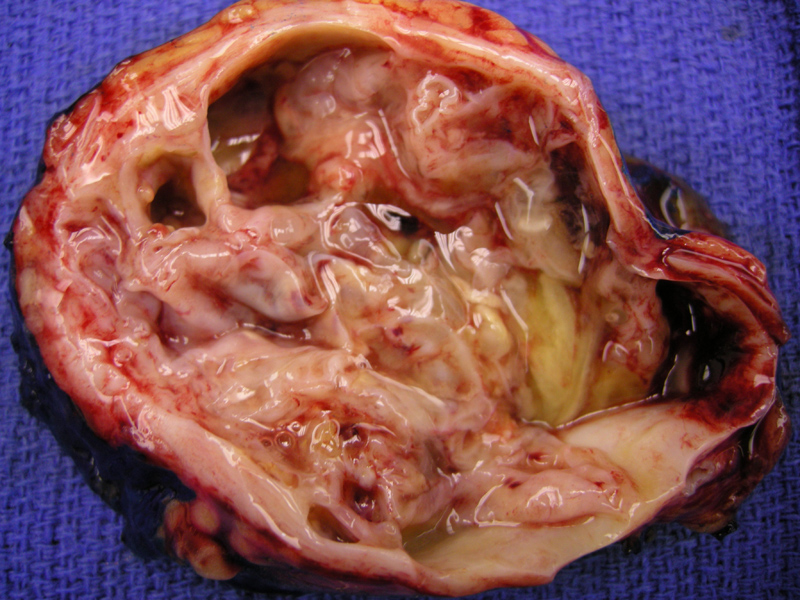
Grossly, the neoplasm is usually multiloculated and contain tenacious mucinous fluid. The lining is smooth and may have papillae or nodules, especially in higher grade cases.
Ultrasound shows a cystic mass containing some solid septated areas.
Papillary fronds are lined by a pleomorphic single cell layer, displaying more complex architecture (compared to a mucinous cystadenoma).
Lower grade dysplasia to upper right, bottom portion demonstrates high grade dysplasia with some intestinal change.
High grade dysplasia can be appreciated (nuclear atypia, nuclear crowding, pseudostratification). Note the ovarian stroma (right)
Smaller cystic glands with necrotic material in lumen and stromal dystrophic calcification are features of high grade dysplasia.
More complex growth into the lumen of the cyst, again, a feature of a higher grade lesion.
MRI of the abdomen shows a rounded heterogenous mass within the tail of the pancreas. The differential includes not only mucinous neoplasms but also solid pseudopapillary neoplasm.
Mucinous cystic neoplasms can be subdivided according to the degree of dysplasia: mucinous cystadenoma (low grade dysplasia), borderline mucinous cystic neoplasm (moderate dysplasia) and mucinous cystadenocarcinoma in situ (high grade dysplasia). Those with an invasive component are termed mucinous cystadenocarcinoma (Fletcher, Weidner).
Grossly, these neoplasms are usually multiloculated and range in size from 2 to 30 cm. Compared to serous microcystic adenomas, the individual locules or cysts are larger. The lining surfcaes are smooth but may exhibit papillary or nodular growths, especially in higher grade cases. The cysts have mucoid fluid. Importantly, unlike intraductal papillary-mucinous neoplasm, these cysts do NOT communicate with the pancreatic ducts.
In the benign mucinous cystadenoma, the lining is composed of a single-layer of columnar epithelium. Increasing intricate architecture (papillary or glandular formation, cellular pseudostratification, crypt invagination) and increasing atypia are features of higher grade lesions. Of inerest, there is "ovarian-type" stroma underlying the epithelial, suggesting that mucinous neoplasms of the pancreas and ovaries may have a common pathogenesis (Weidner). These stromal cells are ER, PR, CD10 and inhibin positive. In very rare cases, the stroma may be sarcomatous. The lining cells are positive for CK 7,8,18,19, EMA and CEA. In contrast, serous cystic neoplasms of the pancreas (also positive for CK 7, 8, 18, 19) are *negative* for CEA (Fletcher).
Occur almost exclusively in women and the majority arise in the body/tail of the pancreas. The most common presentation is a slowly enlarging abdominal mass. Anorexia and weight loss are ominous features and suggest an invasive component. If no invasion is present, however, the prognosis is quite good and surgery is curative.
• Pancreas : Mucinous Cystic Neoplasm
• Pancreas : Solid Pseudopapillary Neoplasm
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 473-4.
Weidner N. Modern Surgical Pathology. Philadelphia, PA: Elsevier, 2003: 894-5.