System: Gastrointestinal: Liver: Autoimmune: Autoimmune Hepatitis

System: Gastrointestinal: Liver: Autoimmune: Autoimmune Hepatitis


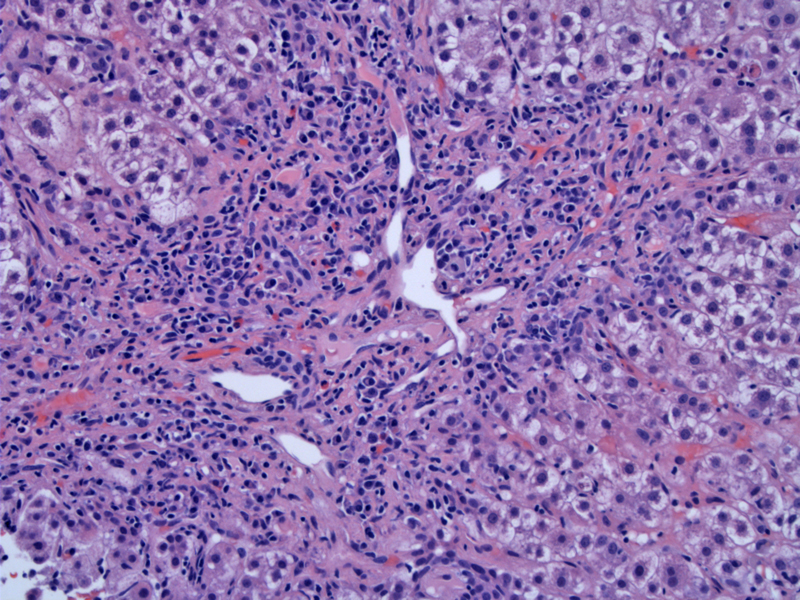
Portal and periportal inflammation with interface hepatitis is typical of autoimmune hepatitis. The necro-inflammatory process may involve the lobules with scattered lymphoplasmacytic aggregates with single cell hepatocytic necrosis resulting in acidophil bodies.
Plasma cells are regarded as the hallmark of this disease. The presence of portal plasma cells in liver biopsies, from patients under therapy-induced remission, has been found to be predictive of relapse following treatment withdrawal. Regenerating hepatocyte rosettes can also be seen here, as clusters of hepatocytes with vacuolated cytoplasm).
Over time, the disease eventuates in a fibrosing process and patients may even present with established cirrhosis.
A different case shows a dense plasma cell spilling out from the portal triad to involve the lobular parenchyma.
Pericentral necrosis is seen here, a feature which not infrequently accompanies the active form of the disease Image
The term autoimmune hepatitis (AIH) describes a heterogeneous group of liver disease characterized by polyclonal elevations of serum immune globulin, circulating autoantibodies, and generally beneficial responses to immunosuppressive therapy. AIH has been observed to occur more frequently in individuals with particular MHC class II alleles, such as DRB1*0301 and DRB1*0401, which share similar amino acid motifs in regions likely to impact peptide binding
Three key histological features are seen in AIH: (1) interface hepatitis (2) prominent plasma cells and (3) regenerative liver cells in rosettes. Significant bridging fibrosis may be found, indicating the chronicity of the disease (Iacobuzio).
Autoimmune hepatitis can be distinguished from primary biliary cirrhosis and primary sclerosing cholangitis as the bile ducts in AIH are preserved (although the lymphocytes may focally invade the bile duct epithelium).
The typical presentation is a woman who presents with insidious onset of lethargy and malaise and during medical evaluation is found to have laboratory abnormalities consistent with chronic hepatitis or even established cirrhosis. Patients often also have arthralgias, myalgias, or oligomenorrhea. A history of autoimmune diseases such as autoimmune thyroiditis, Graves' disease, or ulcerative colitis also may be obtained.
Anti-nuclear antibodies (ANA) are present in about 80% of AIH patients in titers greater than 1:40 and anti-smooth muscle antibodies (ASMA) in titers greater than 1:40 are seen in approximately 70%. The ANA usually demonstrates a homogeneous pattern, due to reactivity against histones and DNA, but other patterns may be seen as well. Other auto-antibodies that may be seen are anti-liver kidney microsomal (anti-LKM), anti-soluble liver antigen (anti-SLA), anti-liver pancreas (anti-LP), anti-asialoglycoprotein (anti-ASGPR) antibodies, and pANCA.
Note that in type 1 AIH, the autoantibodies are either ANA or ASMA; in type 2 AIH, the autoantibodies are anti-LKM and in type 3, the autoantibodies are anti-SLA (Lefkowitch).
Immunosupressive therapy (steroid and azathioprine) has been shown to be effective in reducing mortality from AIH. Liver transplantation is effective in patients with progressive liver disease during or after conventional therapy (Neuberger). Following liver transplantation, incidence of acute rejection is increased modestly, and disease recurrence occurs in some instances.
Patients who have symptomatic AIH with significant biochemical and serologic abnormalities have been found to have approximately a 65% 5-year mortality rate in the absence of treatment (Iacobuzio). Even after highly effective immunosuppressive therapy became the standard of care, patients still exhibit significantly increased mortality relative to that of age-matched controls.
Autoimmune hepatitis demonstrates interface hepatitis with prominent plasma cells.
• Liver : Chronic Hepatitis C Grading (Activity)
Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 559-561
Lefkowitch JH. Anatomic Pathology Board Review. Philadelphia, PA: Elsevier; 2006: 157-8.
Neuberger J., Transplantation for autoimmune hepatitis. Semin Liver Dis (2002) 22 : pp 379-386.