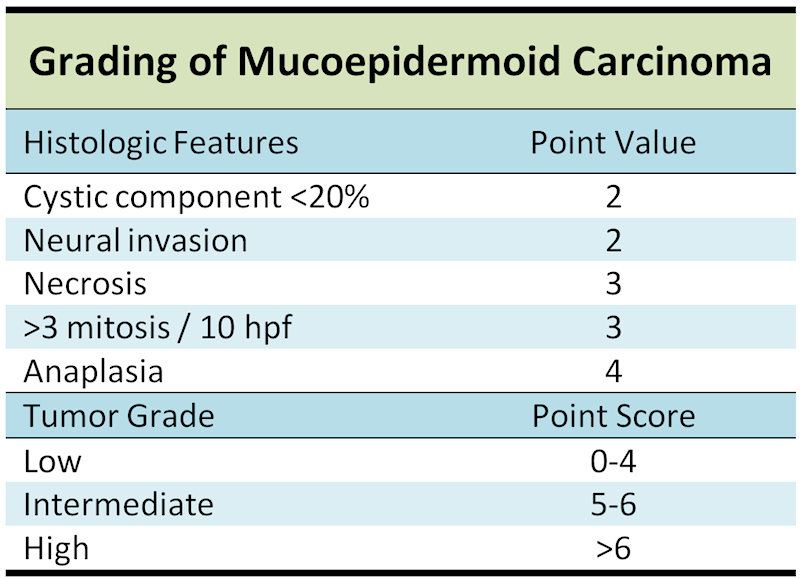
Histologically, MEC is composed of numerous cell types including intermediate cells, epidermoid cells, mucous cells, clear cells and columnar cells in varying proportions, architecture, and differentiation. The appearance of individual tumors vary greatly depending upon the histologic grade. Proposed histologic grading chart for MEC from Goode and Auclair7 , although this is far from universally accepted.
Low grade MEC is predominantly cystic, consisting of variable sized mucin fieled spacec lined by goblet cells.
Some grundgy material fills some cysts- on this power one can see numerous intracystic spaces comprises the majority of the tumor.
Areas of epidermoid cells are found. Note that the proportion of cell types does not correlate with behavior.
The cysts are lined by attenuated cells, some of which are recognizable as mucocytes. Cytological features are relatively bland.
Mucoepidermoid carcinoma(MEC) is a malignant epithelial tumor composed of three cell types: mucous cells, epidermoid cells, and intermediate cells. It is often highly cystic. It is usually classified as low, intermediate or high grade on the basis of histologic tumor features. MEC is the most common salivary gland malignancy in all age ranges, accounting for about 30% of malignant lesions in all salivary glands1 . MEC in children tends to be a low grade neoplasm2 . There is an association with radiation exposure4
MEC typically presents as a solitary painless mass, although higher grade tumors may present with rapid growth and cervical metastasis as well. Clinically, MEC can simulate a benign process such as inflammation, and lesions on the palate can even be fluctuant. There has been noted a slight male predilection (3:2) in MEC affecting the major salivary glands3 . About 9% of tumors arise in the second decade of life. 50-60% of all MECs arise in the major glands (mostly in the parotid gland), 30-40% in the minor glands of the palate, and the rest in the buccal mucosa, lips, retromolar region and tongue5,6 .
For low grade lesions, surgical excision with negative margins is adequate therapy in the absence of known metastatic lesions.
Unlike their high grade counterparts, the low grade MECs rarely recur or metastasize. Recurrence is certainly more likely in the setting of positive surgical margins. Recurrences in the minor salivary glands may arise many years later. Regional metastases for low grade tumors of the minor salivary glands are extremely rare and does not appear to affect overall outcome.
Histological grade of MEC involving the submandibular gland does not correlate with behavior as reliably as for other sites.
Most series show 5-year mortality for low grade lesions 0-3%.
• Salivary Gland : Low Grade Cystadenocarcinoma
• Salivary Gland : Low-Grade Salivary Duct Carcinoma
1 Salivary mucoepidermoid carcinoma: revisited. Luna MA. Adv Anat Pathol. 2006 Nov;13(6):293-307
2 Guzzo M, Ferrari A, Marcom I, et al. Salivary gland neoplasms in children: the experience of the Instituto Nazionale Tumori of Milan. Pediatr Blood Cancer. In press.
3 Guzzo M, Andreola S, Sirizotti G, et al. Mucoepidermoid carcinoma of salivary glands: clinicopathologic review of 108 patients treated at the National Cancer Institute of Milan. Ann Surg Oncol. 2002;9:688–695.
4 Saku T, Hayashi Y, Takahara O, et al. Salivary gland tumors among atomic bomb survivors. Cancer. 1997;79:1465–1475.
5 Spiro RH, Huvos AG, Berk R, et al. Mucoepidermoid carcinoma of salivary gland origin. A clinicopathologic study of 367 cases. Am J Surg. 1978;136:461–468.
6 Auclair PL, Ellis GL. Mucoepidermoid carcinoma. In: Ellis GL, Auclair PL, Gnepp DR, eds. Surgical Pathology of the Salivary Glands. Philadelphia: WB Saunders; 1991;269–298.
7 Goode RK, Auclair PL, Ellis AL. Mucoepidermoid carcinoma of the major salivary glands: clinical and histologic analysis of 234 cases with evaluation of grading criteria. Cancer. 1998;82:1217–1224.