
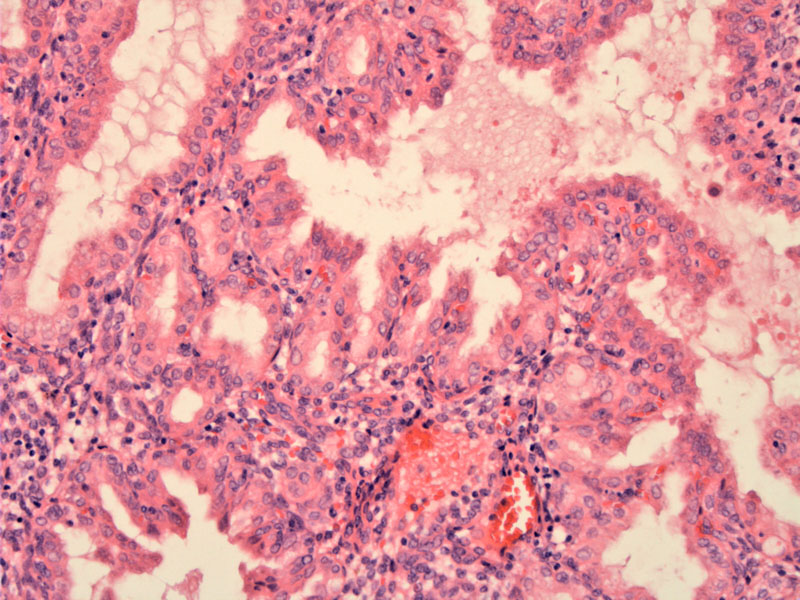
Endometrial biopsy predominantly shows hypersecretory glands thrown into papillary folds consistent with Arias-Stella/gestational endometrium of recent pregnancy
The patient's background endometrium shows pronounced stromal decidualization consistent with recent pregnancy
Trophoblastic cells infiltrating the myometrial muscle fibers are seen as enlarged cells with pleomophic nuclei. Despite the infiltration by trophoblastic cells, the overall architecture is not disturbed. Endometrial glands may be completely engulfed by trophoblastic cells, but there is no necrosis.
In the implantation site, the intermediate trophoblastic cells can have a variable appearance. Here they appear elongated and slightly spindled, whereas in the endometrium, they appear more polygonal. The nuclei when they infiltrate the myometrium are markedly hyperchromatic, with irregular outlines and brighly eosinophilic cytoplasma.
Keratin AE1/3 highlights a benign gland in the center bottom and the infiltrating trophoblastic cells. The immunophenotype of trophoblastic cells is the same as the implantation site intermediate trophoblastic cells in the normal placental site.
Ki-67 is virtually zero consistent with the diagnosis.
The exaggerated placenta site consists of an exuberant infiltration of the myometrium by implantation site intermediate trophoblasts, representing the extreme end of a physiologic process. The distinction between normal placental site and an EPS is somewhat arbitrary because there is no reliable information quantifying the amount and extent of trophoblastic infiltration at different stages of normal gestation.
Intermediate trophoblastic lesions include exaggerated placental site (EPS), placental site nodule (PSN), placental site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor (ETT). Three trophoblastic cell types are recognized: cytotrophoblast, syncytiotrophoblast and intermediate trophoblast.
The EPS can occur in a normal pregnancy or an abortion from the first trimester and is found in approximately 1.6% of spontaneous and elective abortions from the first trimester based on a review of Johns Hopkins cases (Shih).
No specific treatment required.
Resolves after curettage. Those that are not associated with a hydatidiform mole do not carry an increased risk of persistent gestational trophoblastic disease.
• Placenta : Placental Site Trophoblastic Tumor
• Placenta : Implantation Site
• Endometrium : Placental Site Nodule
Shih IM, Kurman RJ. The pathology of intermediate trophoblastic tumors and tumor-like lesions. Int J Gynecol Pathol. 2001 Jan;20(1):31-47.