
Overall, the pathologic diagnosis rests on the following : (i) large tumor cells with deeply eosinophilic cytoplasm, (ii) macronucleoli, and (iii) abundant fibrous stroma arranged in thin parallel lamellae around tumor cells.
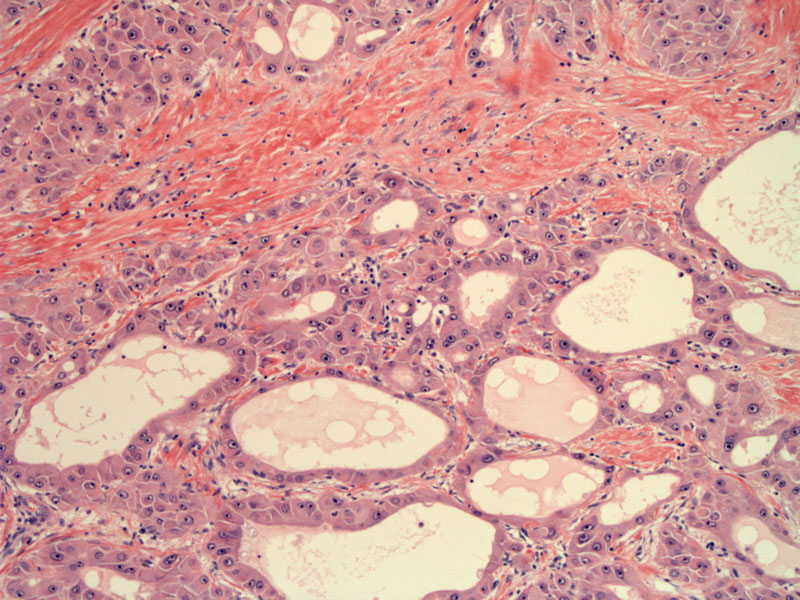
Polygonal cells with eosinophilic cytoplasm form irregular areas of proliferation within a densely fibrotic stroma. Note the parallel (lamellar) arrangement of the collagen bundles.
Another image demonstrates the tumor cells forming solid nests and glandular spaces. The polygonal tumor cells have abundant deeply eosinophilic and granular cytoplasm.
Nucleoli are always prominent in these tumors --and the nuclei often contain vesicular chromatin as you see in this image.
A different case shows the same broad band of lamellar collagen dissecting among haphazard sheets of tumor cells.
These tumor cells are producing bile.
Fibrolamellar hepatocellular carcinoma (FL-HCC) was first described in 1956 by Edmondson (1) as a distinctive form of primary hepatocellular carcinoma. FLHCC differs from HCC in many ways, such as patient demographics, common risk factors, tumor markers, and importantly, prognosis. FLHCC usually occurs in patients without chronic liver diseases such as viral hepatitis and cirrhosis.
Unlike the usual HCC, the background liver is generally noncirrhotic. About 80% of tumors are large, yellow to pale tan in color, well-circumscribed, and heterogenous. The tumor is typically quite large, up to 25cm in diameter. A prominent central scar similar to focal nodular hyperplasia may be present in 75% of cases (Tanaka). The tumor often shows foci of increased vascularity and necrosis.
The average age of patients with FLHCC is ~25 years (Berman) and only 6% are above 50 years of age at the time of diagnosis (Soreide). More than 85% of cases occur in individuals aged ≤35 years, and among the hepatic malignancies in patients aged ≤35 years, 40% were FL-HCC in one series(Craig). In contrast, the average age for HCC is significantly older, at approximately 65 years of age.
Patients may present with common nonspecific symptoms, such as nausea, abdominal discomfort or fullness, weight loss, and night sweats (Liu). Typical presentations may include palpable mass and associated pain in the right upper quadrant. Jaundice may be present in up to 40% of cases. Serum AFP levels may be normal or only slightly elevated.
Successful management of requires early diagnosis to allow for surgical resection with adequate lymph node dissection.
If partial hepatectomy is not feasible because of tumor size or because of its deep extension and adhesion with adjacent organs, liver transplantation should be considered.
The idea that FLHCC has a better prognosis than conventional HCC may be attributable to the following characteristics: its high resectability in most cases, its tendency to occur in young patients, and the absence of associated liver disease. However, the comparative prognosis between FL-HCC patients and patients with HCC without cirrhosis shows no survival advantage (Kakar). In one study, the median survival was 12 months in unresected patients and none survived beyond 5 years, whereas the 5-year survival rate increased to 76% with a median survival of 112 months if the tumors were completely resected (Stipa).
Another large study yielded overall survival rates at 1, 3, and 5 years after surgical resection of 100, 100, and 65% respectively -- for those with liver transplantion, survival rates were 90, 75, and 50% at 1, 3 and 5 years (El-Gazzaz). However, recurrence occurs in about half of the patients within 40 months after receipt of transplant (Starzl).
Berman MA, Burnham JA, Sheahan DG. Fibrolamellar carcinoma of the liver: an immunohistochemical study of nineteen cases and a review of the literature. Hum Pathol 1988;19:784–794.
Berman MM, Libbey NP, Foster JH. Hepatocellular carcinoma: polygonal cell type with fibrous stroma - an atypical variant with a favorable prognosis. Cancer 1980;46:1448–1455.
Craig JR, Peters RL, Edmondson HA et al. Fibrolamellar carcinoma of the liver: a tumor of adolescents and young adults with distinctive clinico-pathologic features. Cancer 1980;46:372–379.
Edmondson HA. Differential diagnosis of tumors and tumor-like lesions of the liver in infancy and childhood. Am J Dis Child 1956;91:168–186.
El-Gazzaz G, Wong W, El-Hadaty MK et al. Outcome of liver resection and transplantation for fibrolamellar hepatocellular carcinoma. Transpl Int 2000;13:S406–S409.
Kakar S, Burgart LJ, Batts KP et al. Clinicopathologic features and survival in fibrolamellar carcinoma: comparison with conventional hepatocellular carcinoma with and without cirrhosis. Mod Pathol 2005;18:1417–1423.
Liu S, Chan KW, Wang B, Qiao L. Fibrolamellar hepatocellular carcinoma. Am J Gastroenterol. 2009 Oct;104(10):2617-24; quiz 2625.
Soreide O, Czerniak A, Bradpiece H et al. Characteristics of fibrolamellar hepatocellular carcinoma. A study of nine cases and a review of the literature. Am J Surg 1986;15:518–523.
Starzl TE, Iwatsuki S, Shaw BW Jr et al. Treatment of fibrolamellar hepatoma with partial or total hepatectomy and transplantation of the liver. Surg Gynecol Obstet 1986;162:145–149.
Stipa F, Yoon SS, Liau KH et al. Outcome of patients with fibrolamellar hepatocellular carcinoma. Cancer 2006;106:1331–1338.
Tanaka J, Baba N, Arii S et al. Typical fibrolamellar hepatocellular carcinoma in Japanese patients: report of two cases. Surg Today 1994;24:459–463
Slides courtesy of Dr. Lida Crooks, Dept of Pathology at VAMC Albuquerque NM.