
Microscopically, one sees dead or dying villi due to the lack of perfusion in the intervillous (maternal) space. Inititally, intravillous hemorrhage occurs followed by collapse of intervillous space as the villi clump together. There is a loss of distinct nuclei of the trophoblasts and they look 'smudgy'. In later phases, pyknosis and karyokrrhexis are seen.
As ischemia progresses, the nuclei of the trophoblasts lose their distinct nuclear morphology - note the smudgy blue-grey indistinct nuclei that meld into the cytoplasm.
Here is a different case demonstrating an older infarct -- there is no nuclear material at all and has a more solidified appearance.
This older infarct shows scattered hemosiderin-laden macrophages and a few residual RBCs.
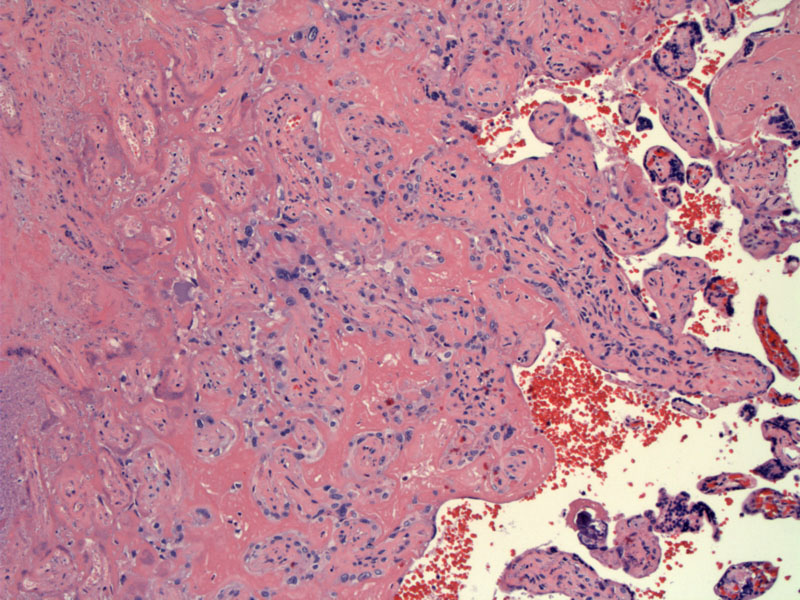
Here's another example of an infarct -- this one is located just under the fetal surface (seen to the right). Note the collapse of intervillous space.
In comparison to the prior image, this image shows loose fibrin from delivery -- this is NOT an infarct.
The edge of another evolving infarct shows consolidation with excessive fibrin but the nuclei are still largely intact.
As one moves closer to the more established infarct, one can appreciate the transition to loss of nuclear viability.
The vascular background remains intact in this early infarct.
A distinct area of pallor is seen here in the parenchyma consistent with an established infarct.
A placental infarct occurs when maternal blood flow through the spiral arteries is compromised, leading to ischemic necrosis of the villi. Infarcts smaller than 3cm in diameter near the edge of the placenta are extremely common and are of little clinical significance. These small infarcts are most likely atrophy of placental tissue rather than true infarcts, although the histologic features are identical.1
More concerning are multiple infarcts distributed throughout the placenta, large infarcts and centrally located infarcts prior to term -- these infarcts indicate reduced uteroplacental blood supply and may be associated with other gestational abnormalities. In pre-term infants (first or second trimester), the placenta should not contain any infarcts and if present, signify some sort of pathologic process such as pre-eclampsia. Infarcts involving greater than 50% of the placenta may lead to severe hypoxic injury and fetal demise -- infarcts are especially damaging to small placentas (below the 10th percentile in size).1,2
Grossly, the appearance of infarcts may differ depending on the age of the infarct. Older infarcts are yellow, grey-tan, white and firm. Younger infarcts are dark red, congested and may be difficult to distinguish from normal placental tissue. However, all infarcts should feel firmer than surrounding tissue -- and it may be best to place the placenta in formalin to better view younger infarcts.1,2
There is an association between placental infarcts, maternal hypertension, pre-eclampsia and maternal thrombophilias (ie. lupus anticoagulant). Large infarctions may be associated with fetal compromise.
1 Kraus TK, Redline RW, Gersell DJ. Placental Pathology: Atlas of Nontumor Pathology.First series, Fascicle 3. Washington DC: AFIP; 2004: 123-5.
2 Baergen RN. Manual of Benirschke and Kaufmann's Pathology of the Human Placenta. New York, NY: Springer; 2005: 472-3.