
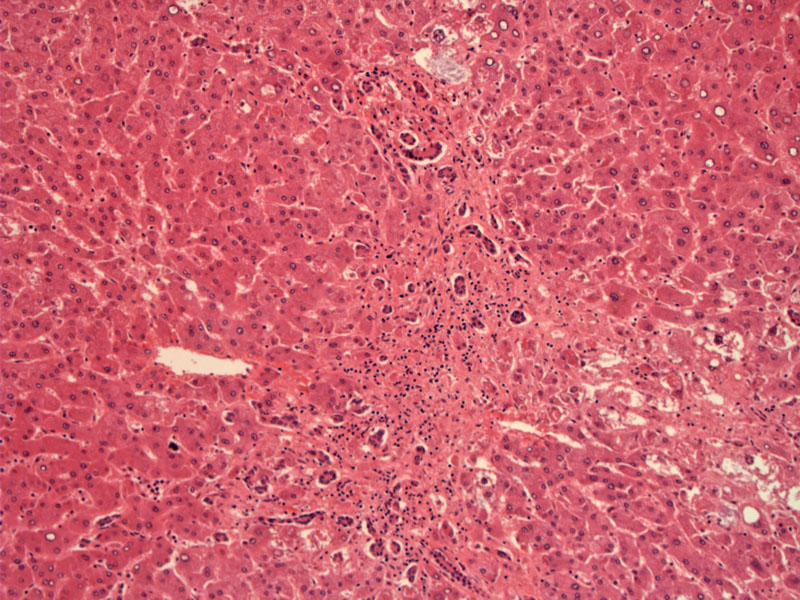
Toxicity resembles alcoholic hepatitis, with Mallory bodies, ballooning degeneration, and hepatitis with a neutrophilic infiltrate. This case, however, shows a prominent bile ductular proliferation.
Reactive multinucleated cells are seen, and Mallory hyaline is found as in alcoholic hepatitis. Some of the hepatocytes show foamy change, which is due to drug accumulation.
Nonalcoholic steatohepatitis (NASH) is a common cause for liver disease and is often attributed to metabolic syndrome, however, drug-induced steatohepatitis ought to be in the differential in the right clinical setting. Chronic use of amiodarone has been shown as an independent cause of steatohepatitis. Other commonly used drugs such as tamoxifen and corticosteroids are thought to exacerbate underlying steatohepatitis (Stravitz).
Amiodarone is a lipophilic drug that concentrates in the liver and over a period of time leads to hepatotoxicity. It is used in the treatment of ventricular arrhythmias resistant to conventional therapy. It has several potentially serious side effects, including progressive liver disease, pulmonary fibrosis, neurotoxicity, ocular complications, and thyroid dysfunction. Up to 80% of patients chronically administered amiodarone will experience side effects.
There is significant histological similarity between amiodarone-induced liver disease and alcoholic and nonalcoholic steatohepatitis (Raja).
Amiodarone hepatotoxicity usually presents with asymptomatic elevation of liver enzymes, generally showing a mild mixed hepatitic-cholestatic pattern, with normal bilirubin. Elevated enzymes can develop between several weeks to years after initiation of the drug. Overall, the drug causes elevated liver enzymes in up to 30% of patients and steatohepatitis in 1–2%.
Liver enzymes should be measured at baseline and at 3 to 6 month intervals for patients receiving doses less than 400 mg/d, and more often with higher doses.
Liver injury reverses on discontinuation of the drug, or dose reduction, but may be delayed weeks or months. In some instances, steatohepatitis can lead to cirrhosis, portal hypertension and other complications of liver failure.
→The classic findings in alcoholic and non-alcoholic steatohepatitis (steatosis, ballooning degneration, lobular inflammation, fibrosis) are seen in amiodarone-induced steatohepatitis as well.
Raja K, Thung SN, Fiel MI, Chang C. Drug-induced steatohepatitis leading to cirrhosis: long-term toxicity of amiodarone use. Semin Liver Dis. 2009 Nov;29(4):423-8. Epub 2009 Oct 13.
Stravitz RT, Sanyal AJ. Drug-induced steatohepatitis. Clin Liver Dis. 2003 May;7(2):435-51.