
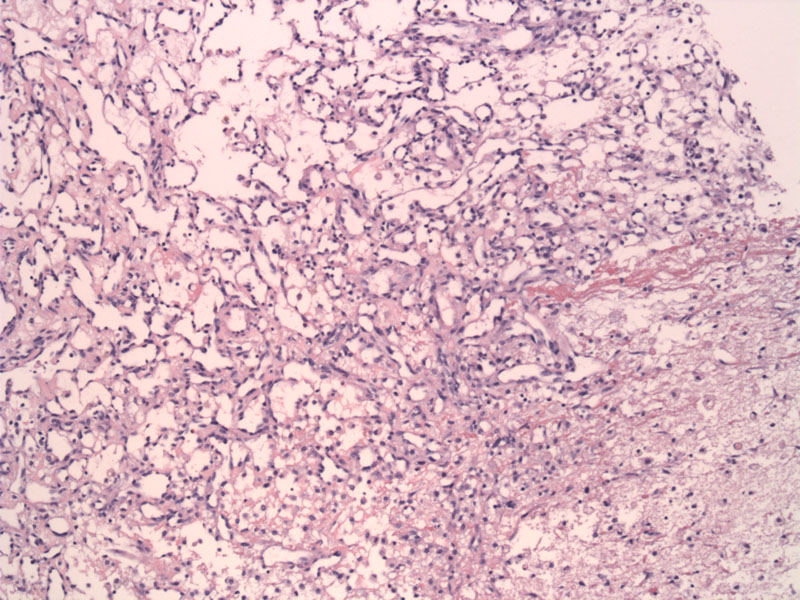
Angiosarcoma is made up of anastomosing, irregular vascular channels which diffusely infiltrates the breast parenchyma. Note that low-grade angiosarcomas may be virtually indistinguishable from hemangiomas, therefore, several clues may be helpful. Benign tumors are usually less than 2 cm, and the endothelial cells lining the channels are flat and non-proliferative.
The vascular spaces are lined by flat endothelial cells with enlarged hyperchromatic nuclei and occasional mitotic figures (not clearly shown here).
Higher-grade features include a solid spindled-cell architecture, endothelial tufting, prominent cytologic atypia of endothelial cells, large vascular cisterns (blood lakes), areas of hemorrhage and necrosis. This image demonstrates more of an intermediate grade tumor.
An image demonstrating large dilated vascular spaces which appear deceptively bland, but are surrounding normal breast epithelial units. Despite the bland appearance of the cells, the infiltrative and anastamosing nature of the vascular spaces is clearly indicative of malignancy.
The endothelial cells lining the vascular channels may have a hobnailed appearance (naked nuclei protruding into the lumen). These areas are more easily recognizable as malignant than the previous image.
Angiosarcoma shows other deceptively bland areas but islands of such vascular spaces, with tufting, within the adipocytes is a clue to their malignant nature.
Angiosarcomas show strong staining by vascular markers such as CD34 and CD31. This stain really highlights the anastamosing network which is a defining hallmark of this tumor. Although not shown here, a Ki-67 stain can be used to demonstrate proliferative activity, as normal endothelial cells should have a proliferation rate less than 0.1%.2
By contrast, this angiosarcoma is high grade and lacks overt vasoformative features in many areas.
Angiosarcomas are rare, but represent the most common sarcoma in the breast. There is a bimodal distribution, with the tumor arising de novo in younger women in their 30s, and arising in older women as a consequence of radiation for breast cancer. Approximately 0.1% of patients receiving breast radiation develop angiosarcomas 2-10 years after radiation treatment.1 Most of these lesions arise in the skin or subcutaneous fat (in the site of the radiation field), with only a minority affecting the deeper breast parenchyma.
Another more aggressive form of angiosarcomas occur as a rare complication lymphedema secondary to radical mastectomy. These lesions, termed Stewart-Treves syndrome generally arise in the arm, which is the site most commonly affected by lymphedema. These lesions are high-grade and spread quickly throughout the body as a solid or papillary growth of undifferentiated cells, with an bleak prognosis1
An important feature to remember is that the periphery of angiosarcomas can often appear low-grade (identical to benign hemangiomas), while higher-grade areas may be 'hidden' in other areas of the tumor. Therefore, thorough sampling is imperative.
In younger women (de novo tumors), the lesion presents as a painless mass in the breast parenchyma, and bilaterality is common. In post-radiation induced angiosarcomas, they are generally more superficial and initially appear as a purple discoloration of skin. The tumor may or may not involve the deeper breast parenchyma.
Surgery; role of chemotherapy is not yet clear.
Highly dependent on grade of tumor. 5 year survival of low, intermediate and high-grade tumors are 76%, 70% and 15% respectively.2 High-grade lesions have a propensity to metastasize to the contralateral breast, liver and lung.
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 956-8.
2 O'Mallye FP, Pinder SE. Breast Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2006:289-294.