
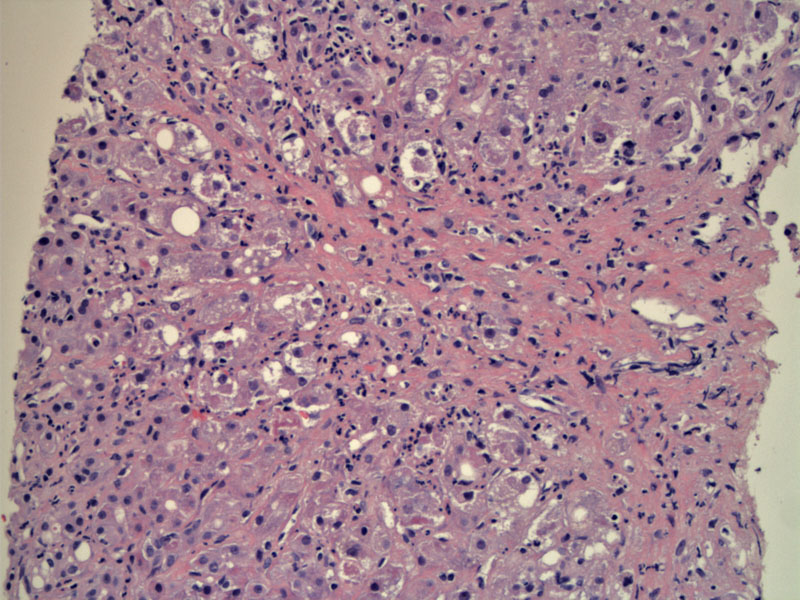
Cellular swelling, spotty necrosis, and Mallory bodies with a variably intense neutrophilic infiltrate are seen.
Note the presence of Mallory hyaline (arrow), which are eosinophilic tangles of intermediate filaments inside degenerating hepatocytes. Mallory hyaline is not entirely unique to alcoholic liver disease, as it may also be recognized in cases of non-alcoholic fatty liver disease, chronic cholestatic liver disease, copper toxicity, and amiodarone toxicity.
Prominent Mallory bodies and ballooning degeneration (enlarged, hydropic cells with granular cytoplasm) can be appreciated.
Some cells demonstrate pigmentation (see center cell), which can either be cholestasis or hemosiderin (iron) deposition in hepatocytes.
Dense pericellular fibrosis has developed here, which indicates a more advanced disease progress than simple alcoholic hepatitis. The trichrome stain highlights the end result of deposition of collagen in the spaces of Disse along the central zone sinusoids. Eventually, this fibrosis extends, and central zones and portal tract become incorporated in the same scar, and beginning division of the micro-anatomy into smaller sub-units. Continued progression of this process is the basis for alcoholic cirrhosis.
Alcohol hepatitis can eventually lead to cirrhosis. Fibrous bands can be seen (right image) bridging between portal triads.
Alcohol abuse is estimated to affect more than 14 million Americans. The effects of alcohol on the liver can be divided into three categories: hepatitis steatosis (fatty change), alcoholic hepatitis and cirrhosis. These changes do not necessarily represent a continuum. For example, hepatitis steatosis and alcoholic hepatitis can occur concurrently or independently. However, cirrhosis is usually preceded by these two changes. Hepatic steatosis is fully reversible if alcohol consumption is discontinued. Alcohol hepatitis can resolve slowly -- or progress to cirrhosis if alcohol abuse continues. Note that 10-15% of alcoholics (overall) develop cirrhosis.1,2
Fatty liver change can occur after just modest consumption of alcohol. Initially, small lipid drop droplets (microvesicular) are seen in the hepatocytes -- with increased alcohol intake, larger fat droplets are seen (macrovesicular) which may push the hepatocyte nucleus to the periphery of the cell. Grossly, the liver is enlarged, fat and greasy -- on a tangent, this is which is why ducks are forced-fed a fatty diet to make 'foie gras'.
Alcoholic hepatitis consists of the following four histopathological changes:
(1) Ballooning degeneration and necrosis -- hepatocytes are swollen with granular or clumped cytoplasm; apoptotic bodies may be present.
(2) Mallory hyaline -- clumps of intermediate filaments form eosinophili inclusions, usually in degenerating hepatocytes. Note that Mallory hyaline is not pathognomonic for alcoholic hepatitis, but can also be seen in Wilson disease, primary biliary cirrhosis, cholestasis and hepatocellular tumors.
(3) Neutrophilic infiltrate -- neutrophilics will be present, commonly clustered around the ballooned and degenerating hepatocytes, especially those containing Mallorys hyaline.
(4) Fibrosis -- strands of collagen will envelope hepatocytes in a 'chicken wire' pattern. Fibrosis starts around the sinusoids (in the space of Disse) and zone 3 (centrilobular) areas, eventually, progressing to bridging fibrosis and micronodular cirrhosis. Ito cells (perisinusoidal stellate cells) and portal tract fibroblasts are stimulated to synthesize collagen by the toxic effects of alcohol, leading to perisinuosidal fibrosis -- the very beginnings of cirrhosis.1,2
Although fatty change is largely asymptomatic with perhaps mild elevations of liver function tests (LFTs), patients with alcoholic hepatitis have a variable presentation, ranging from malaise to coma and death. Alcoholic hepatitis classically presents with weight loss, fever, tender hepatomegaly and jaundice. Liver enzymes are elevated (AST >> ALT) as well as increased bilirubin (hyperbilirubinemia). Some patients give a history of binge drinking.
Treatment is focused largely on abstinence. For abstinent patients who have established cirrhosis, the possibility of transplantation is an option. American Society of Gastroenterology recommends corticosteroids for severe alcoholic hepatitis.
The course of alcoholic hepatitis is unpredictable. In some patients, abstinence may lead to complete resolution of the disease. Other patients will develop cirrhosis despite abstinence. Furthermore, each episode of alcoholic hepatitis carries a 10%-20% risk of death.1
1 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 904-7.
2 Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 534-7.