System: Gastrointestinal: Colon: Infectious: Pseudomembranous Colitis

System: Gastrointestinal: Colon: Infectious: Pseudomembranous Colitis


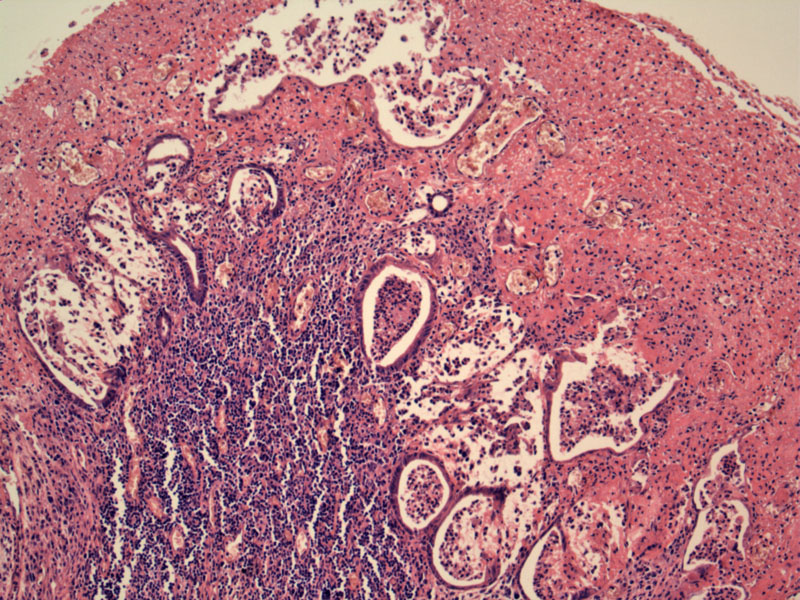
A fibrinopurulent cap overlies dilated, simplified and injured colonic glands with crypt abscesses.
A mushroom-like eruption arises from the dilated crypts. Note the dense inflammatory infiltrate in the lamina propria.
A larger mushroom cloud of fibrinous exudate erupts from ballooned glands. This pseudomembrane is mainly composed of mucus, fibrin and neutrophils.
Another image of glands 'erupting'. The dilated glands contain fibropurulent debris and an attenuated lining.
Here is a different case, with a flatter morphology (not an actual mushroom cloud) but with the same injury pattern.
1 Image
2 Image
3 Image
glands dilate as they Image
some more tubular retention Image
exudate Image
iamge Image
Clostridium difficile pseudomembranous colitis (PMC) is responsible for approximately 3 million cases of diarrhea and colitis annually in the United States. Pseudomembranous colitis is named after the white plaque-like lesions that adhere to a reddened and friable bowel mucosa. These plaques tend to bleed when scraped. These plaques are not true membranes since they do not contain epithelium (but rather, fibrinopurulent debris), but only appear so grossly.
Microscopically, PMC displays a striking 'volcano' or 'mushroom cloud' morphology. The epithelium is denuded -- intercrypt necrosis and a dense infiltrate of neutrophils are seen in the lamina propria. Most notably, a cloud or eruption of fibropurulent debris appear to extrude from the ballooned crypts. Basically, it looks like an atomic bomb was detonated.
C. difficile infection generally occurs after orally administered antibiotics because this organism cannot establish its presence in normal gut flora. Antibiotics most frequently associated with this infection include clindamycin, ampicillin, amoxicillin, and cephalosporins. Patients tend to be elderly, although all ages can be affected. Initially, the patient usually experiences watery diarrhea, abdominal cramps, fever and leukocytosis -- bloody diarrhea may be seen. The range of presentation varies from mild diarrhea to fulminant disease with toxic megacolon and perforation.2 The diagnosis can be confirmed using an enzyme immunoassay for C. difficile toxins A and B with results available in two to four hours.
Antibiotics (oral Metronidazole or Vancomycin) and supportive measures. Fulminant colitis develops in approximately 1% to 3% of patients, with toxic megacolon, perforation, and even death.
Approximately 15% of patients experience relapse after initial therapy and require retreatment, often with an extended, tapering regimen. The level of anti-toxin antibody in the serum is inversely associated with severity of disease and risk for relapse.
• Small Intestines : Enteritis necroticans (Pigbel)
1 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 837
2 Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 278-282.