System: Skin: Dermis: Neoplastic: DFSP, Nodular Variant

System: Skin: Dermis: Neoplastic: DFSP, Nodular Variant


Author: Corinne Stephenson
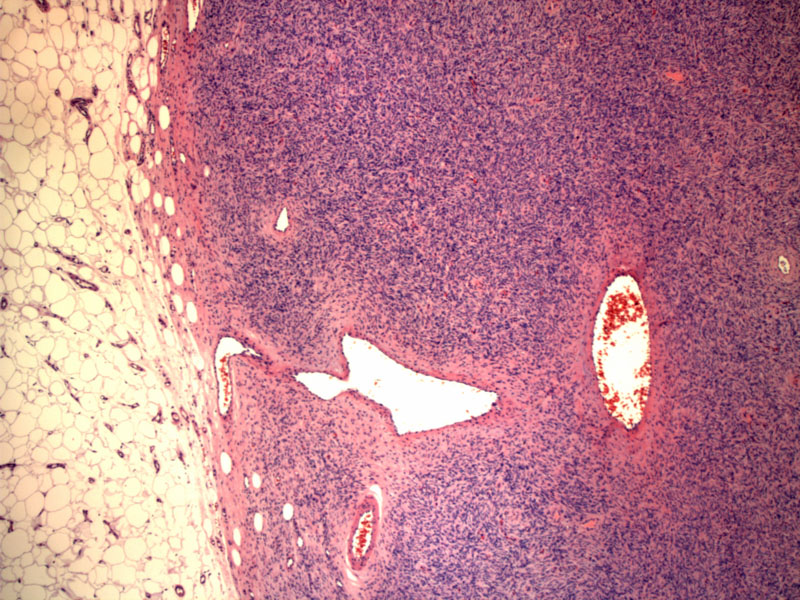
The periphery of the lesion shows Image
At intermediate power, the cells form a recognizable storiform, or pinwheel,arrangement. Image
DFSPs have characteristically strong staining for CD34. Image
Dermatofibrosarcoma protuberans (DFSP) is a malignant subcutaneous fibrous tissue tumor. It is slow-growing, locally aggressive and can metastasize (though this rarely occurs). Even after wide excision, about 20% recur (Garcia). When they recur, they tend to show up as just another DFSP, as opposed to transforming into something more sinister like a fibrosarcoma. If transformation occurs, the tumor is considered more aggressive with a higher probability of metastasis.
The histologic appearance of DFSPs is characterized by a poorly circumscribed dermal proliferation of spindled cells which extends into the subcutis. The dermal infiltrate is usually separated from the normal-appearing epidermis and can be quite cellular, creating pinwheel or storiform patterns which can be seen at low to intermediate power. A helpful feature is found on the periphery of the lesion - so-called "honeycombing" which occurs when the lesional cells wrap around the adipocytes of the subcutaneous tissue. The cells do not demonstrate significant atypia or numerous mitoses.
DFSPs are strongly positive for CD34. Should they contain any areas of fibrosarcomatous transformation, these areas will lose their CD34 positivity.
The relatively recent discovery of a recurring translocation resulting in a novel fusion protein has led to additional treatment options for DFSP (discussed below).
DFSPs are most commonly found on the trunk or proximal extremities of young and middle-aged adults. The clinical appearance is characterized by an indurated plaque with one or more cutaneous nodules.
Because DFSPs are so infiltrative and tend to recur, wide excision is the preferred surgical option. However, Mohs micrographic surgery is being increasingly used, especially in cosmetically sensitive areas, though there is debate as to the ability of using immunohistochemistry on frozen tissue to confirm negative margins. Recent studies have shown that Mohs is equal or better than wide excision, though the number of cases is relatively low (Parisi).
The translocation of the COL1A1 gene on chromosome 17 to the PDFGRBeta gene on chromosome 22 is a recurring genetic defect in DFSPs and results an increased amount PDFGRBeta protein, as demonstrated by FISH. Though the exact mechanism of this novel fusion protein is not completely understood, clinicians are turning to tyrosine-kinase inhibitors such as imatinib to try and combat aggressive, recurrent or metastasized DFSPs by silencing the downstream effects of this aberrant PDFGRBeta protein.(Sundram)
The prognosis for conventional DFSPs is very good, though, as mentioned before, local recurrence can be an issue. Fibrosarcomatous transformation can portend a poorer prognosis.
McKee PH, Calonje E, Granter S. Pathology of the Skin with Clinical Correlations. 3rd Ed. Philadelphia, PA: Elsevier; 2005: 1729-1734
Patterson JW, Wick MR. Nonmelanocytic Tumors of the Skin.4th Series. Washington, DC: American Registry of Pathology; 2006: 217-221.
Weedon D, Strutton G. Skin Pathology.2nd Ed. London, England, UK: Elsevier; 2002: 934-936
Garcia JJ, Folpe AL. The Impact of Advances in Molecular Genetic Pathology on the Classification, Diagnosis and Treatment of Selected Soft Tissue Tumors of the Head and Neck. Head and Neck Pathol.2010;4:70-76.
Sundram UN. Dermatofibrosarcoma Protuberans:Histologic Approach and Updated Treatment Recommendations.Clinical Advances in Hematology and Oncology. 2009;7(6):406-408
Paradisi A, Abeni D, Rusciani A, et al. Dermatofibrosarcoma protuberans:wide local excision vs. Mohs micrographic surgery. Cancer Treat Rev. 2008;34:728-736.