
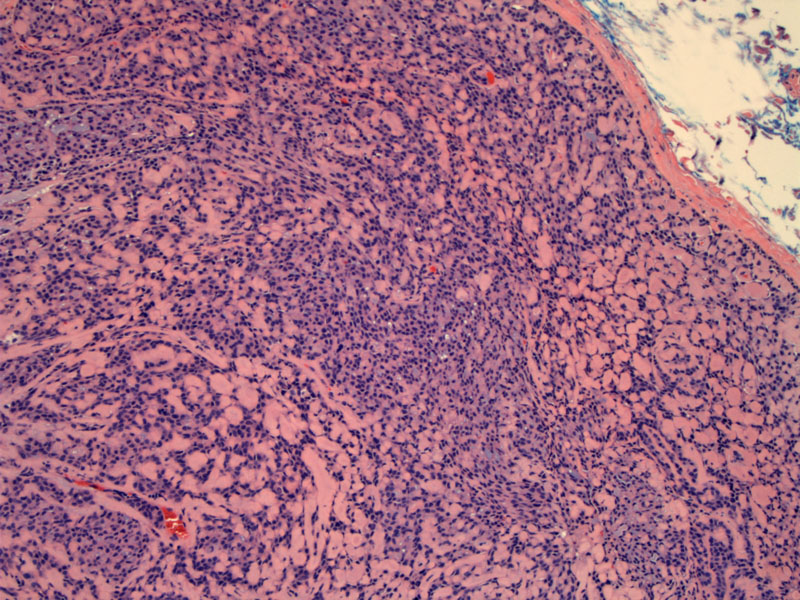
Basal cell adenomas of the major salivary glands are well encapsulated as seen here. In the minor salivary glands, the tumor may be unecapsulated (Brandwein).
At higher power, excessive balls of eosinophilic basement membrane can be appreciated.
The nuclei of the basaloid cells are pushed to the periphery from the elaboration of abundant hyaline material
Tumor capsule interfaces with normal parotid (bottom image).
There is variable 1-2+ c-kit staining in this BCA. C-kit expression is seen in adenoid cystic carcinoma, polymorphous low grade adenocarcinoma and monomorphic adenomas and thus, is not useful in distinguishing between these three entities (Edwards).
Focal variable 2+ SMA highlights the myoepithelial (peripheral or abluminal basaloid).
Keratin AE1/3 highlights the epithelial (luminal) component.
Aspiration of this lesion shows aggregates of basaloid cells.
PAS highlights the abundant hyaline basement membrane material.
Basal cell adenoma is a subtype of monomorphic adenoma that is uncommonly seen and represents only about 2% of salivary gland tumors (Brandwein). About 70% arise in the parotid glands and 10-20% in the upper lip.
Like pleomorphic adenomas, these tumors typically present as discrete, mobile, non-painful masses. There are four main histologic subtypes: solid, trabecular, tubular and membranous.
The membranous subtype of basal cell adenoma, also known as a dermal analogue tumor, is a distinct variant morphologically similar to cylindromas (cutaneous adnexal tumors). In contrast to the other histologic subtypes which are solitary, membranous BCA grow in a multifocal and multinodular fashion.
This membranous basal cell adenomas may be seen in the context of the autosomal dominant salivary gland-skin adnexal tumor syndrome, a.k.a. Brooke-Spriegler syndrome. Patients develop hundreds of dermal cylindromas ("turban tumor"), trichoepitheliomas, eccrine spiradenomas as well as similar tumors in the salivary gland. The culprit germline mutation involves CYLD (cylindromatosis gene), a tumor suppresor gene located at chromosome 16q12-q13 (Yu, Fletcher).
Membranous adenomas usually arise in the parotid. Basal cell carcinomas generally arise in the 7th decade with a 2:1 female predilection. However, membranous adenomas have an equal gender distribution.
Paroditectomy with preservation of the facial nerve is the treatment of choice for this lesion. There is has been reportedly a higher rate of recurrence associated with the membranous subtype of this tumor due to its multifocal nature (Brandwein, Fletcher).
• Salivary Gland : Basal Cell Adenoma, Trabecular Type?
• Salivary Gland : Basal Cell Adenoma, Solid Type
Brandwein-Gensler M. Head and Neck: Illustrated Surgical Pathology Series. New York, NY: Cambridge University Press; 2010: 286-293.
Edwards PC, Bhuiya T, Kelsch RD. C-kit expression in the salivary gland neoplasms adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and monomorphic adenoma.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003 May;95(5):586-93.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 255-7.
Yu GY, Ubmüller J, Donath K. Membranous basal cell adenoma of the salivary gland: a clinicopathologic study of 12 cases. Acta Otolaryngol. 1998 Jul;118(4):588-93.