
The vessels show profound eosinophilic waxy acellular thickening indicative of involvement by amyloid. Vascular involvement makes the vessels fragile, potentially resulting in mucosal petechial hemorrhage and/or ischemic changes
The surface epithelium shows chronic injury changes including marked glandular dropout. The epithelium may even become ulcerated and mimic chronic inflammatory bowel disease.
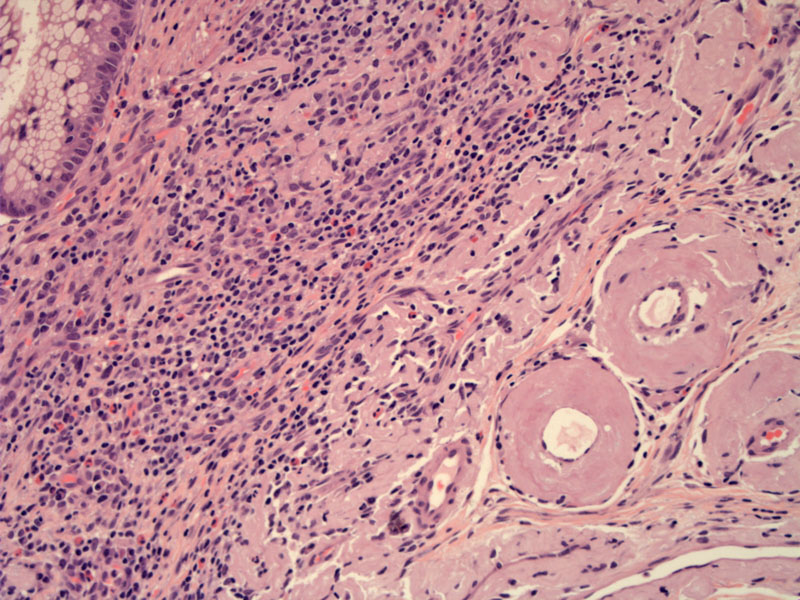
Amyloid insinuates between the fibers of the muscularis propria. This finding is associated with GI motility disorders.
The muscularis is disrupted by waxy deposits of amyloid but also chronic inflammation. The AL amyloid type is the more frequent to show this pattern of deposition in the muscularis and medium sized vessels.
Another patient shows a nodular deposit of amyloid in the immediate submucosa.
Gi involvement is frequent in all types of systemic amyloidosis,
Colon involvement by amyloidosis can mimic other diseases such as IBD, ischemic colitis, collagenous colitis, and even malignancy. Endoscopically, one may encounter polypoid lesions, ulcerations, nodules, or diffusely distributed petechial mucosal suggillations (Ebert). Complications are important and range from colonic dilatation, pseudo-obstruction, stricture, volvulus, and perforation.
For those with underlying AL amyloidosis, the goal is to suppress the synthesis of immunoglobulin light chains by controlling the underlying plasma cell disorder with chemotherapy. For AA amyloidosis, chlorambucil and inhibitors of tumor necrosis factor (TNF)-alpha for inflammatory arthritis may induce regression of amyloid deposits.
Patients with pseudo-obstructive symptoms have a grave prognosis. Survival for those with AL amyloidosis is on the order of 2 years.
• Spleen : Splenic Amyloidosis
Ebert EC, Nagar M. Gastrointestinal manifestations of amyloidosis. Am J Gastroenterol. 2008 Mar;103(3):776-87.
from VA box