
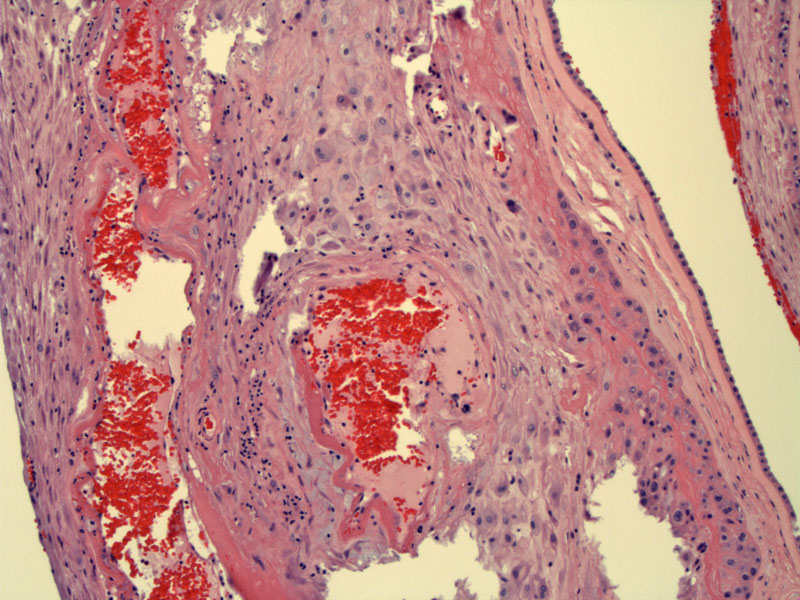
Fetal membranes are seen on the right and a clearly vasculopathic vessel is seen in the maternal decidua.
Fibrinoid necrosis and atherosis (foamy macrophages in vessel wall) can be appreciated. Fibrinoid necrosis is more frequently seen in decidual vasculopathy than atherosis.
Mild decidual vasculopathy as demonstrated by a thin rim of fibrinoid necrosis.
Chronic inflammatory cells can be seen in the vessel wall and surrounding decidua. Note the deeply eosinophilic material in the vessel wall (fibrinoid necrosis).
Zones of acellular eosinophilic material and so-called ghost villi consistent with placental infarcts are seen here. Approximately 1/3 of placentas from preeclamptic women also demonstrated zones of infarction (Zhang).
Note that some examples of decidual vasculopathy may appear subtle. This example shows only increased perivascular eosinophilia but is indicative of this condition all the same.
Preeclampsia affects approximately 7-10% of pregnancies. There are many placental histological findings which are nonspecific to this condition, but material vasculopathy appears to be a direct consequence and thus, is considered highly specific. In one large study, approximately 25% of placentas from women with preeclampsia showed decidual vasculopathy. These changes (defined as maternal vascular atherosis and fibrinoid arterial medial necrosis) were more frequently found in smaller placentas, earlier gestational age complicated by preeclampsia (<30 weeks gestation) and primigravid women.1
Under normal circumstances, trophoblasts from the placenta infiltrate the arteriole walls of the decidua and superficial myometrial vessels, replacing them fibrinoid. Thus, the vessels become rigid, large, open and unresponsive to vasoactive mediators. This is obviously beneficial in establishing protected blood flow in the placenta. In preeclampsia, the invasion of trophoblast is only superficial and fails to invade a large portion of the decidua and proximal myometrium. Thus, these vessels fail to 'convert' and retain their muscular wall and small lumens. This pathologic process is term lack of physiologic conversion.
Other changes found in decidual vasculopathy include: (1) atherosis - foamy macrophages within the vessel wall; (2) vascular thrombosis due to endothelial damage; (3) fibrinoid necrosis of the media - not to be confused with the physiologic deposition of fibrinoid; (4) decidual vasculitis - chronic inflammation of the decidual vessels and surrounding decidual tissue; (5) decidual necrosis is often seen as well.2 c
1 Zhang P, Schmidt M, Cook L. Maternal vasculopathy and histologic diagnosis of preeclampsia: poor correlation of histologic changes and clinical manifestation. Am J Obstet Gynecol 2006 Apr;194(4):1050-6.
2 Baergen RN. Manual of Benirschke and Kaufmann's Plathology of the Human Placenta. New York, NY: Springer; 2005: 119, 333-7.