
Immature neuroepithelium forms primitive tubules (lower image).
Another image of immature neural tissue forming a tubule -- the surrounding tissue may be a blend of glial fibrillary background and primitive mesenchyme.
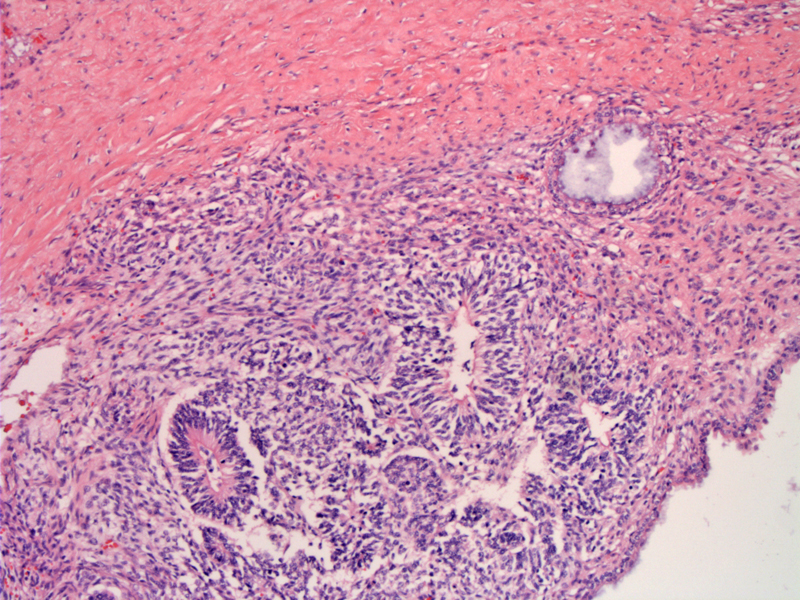
Immature mesenchyme is seen surrounding poorly-formed glandular structures.
Another area with a haphazard arrangement of glands surrounded by primitive mesenchyme. Note the cystically dilated gland on the upper left. Immature neural elements are not as obvious here.
Here is an area of immature mesenchymal tissue. There may be hints of immature neural tissue condensing to form tubules in the center.
Immature mesenchymal stroma is hypercellular with hyperchromatic spindle cells.
Immature teratomas are the third most common malignant germ cell tumor (following dysgerminoma and yolk sac tumor).
Grossly, the tumor is unilateral, solid and bulky (average of 18 cm in diameter) -- a smaller cystic component is often present. The capsule is ruptured in 50% of cases. A dermoid cyst containing hair, keratinous debris, bone and cartilege may be found within the immature teratoma in 25% of cases. A benign cystic teratoma may be in the contralateral ovary in 10-15% of cases.1,2
Microscopically, the tumor is composed of a haphazard mixture of mature and immature teratomatous elements. The easiest immature element to identify is neuroepithelium in the form of columnar embryonal cells with hyperchromatic nuclei forming rosettes and tubules. Other immature elements include immature epithelium, cartilege or mesenchyme.2
Grading of immature teratomas depends on the amount of immature neuroepithelium.
- Grade 0: contains no immature neural elements.
- Grade 1: less than 1 low power field (40x objective) per slide
- Grade 2: 2-3 lpf/slide
- Grade 3: 4+ hpf/slide
Note that by definition, immature teratomas must be grade 1-3 since they have to contain some immature neuroepithelium, however, a grade 0 metastases containing only mature elements can arise out of an immature teratoma of any grade.2
S-100 may be helpful in highlighting the neural elements. Glia will stain with GFAP (glial fibrillary acidic protein) and neuroepithelial cells will stain with NSE (but not usually GFAP).2
In some instances, the neuroepithelial components differentiate into tumors similar to those found in the central nervous system. The three most commonly seen patterns are: primitive neuroectodermal tumors, glioblastoma multiforme and ependymoma. These entities are either classified as monodermal immature teratomas or variants of immature teratomas.2
Most common in the first two decades of life (average age at diagnosis is 18). Symptoms are nonspecific and patients may present with abdominal pain, swelling and sometimes a palpable mass. Serum AFP levels are elevated, but significantly lower than in yolk sac tumors. 90% of patients have mildly elevated CA-125 and 50% of patients have elevated CA 19-9. Some patients may have a history of a previous mature teratoma that had ruptured.1
Most patients can be treated with a unilateral oophorectomy and biopsies of all visible peritoneal implants. For advanced grade or stage tumors, adjuvant therapy with VAC (vincristine, dactinomycin, cyclophosphamide) is recommended.
The majority (50-80%) of patients are Stage I at the time of diagnosis. These tumors spread by implantation (gliomatosis peritonei) in the peritoneum and omentum. The histology of the extra-ovarian implants is significant. Mature implants do not affect outcome, whereas immature implants carry a worse prognosis. There have been 3 reported cases of glioblastoma multiforme arising from peritoneal gliomatosis.3
Postchemotherapy regression of immature teratoma implants to mature teratoma implants has been observed.
• Ovary : Mature Cystic Teratoma
• Peritoneum : Gliomatosis Peritonei
1 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 531-5.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 609-612.
3 Gallion H, van Nagell JR Jr, Donaldson ES, Hanson MB, Powell DF. Immature teratoma of the ovary. Am J Obstet Gynecol. 1983 Jun 15;146(4):361-5.