
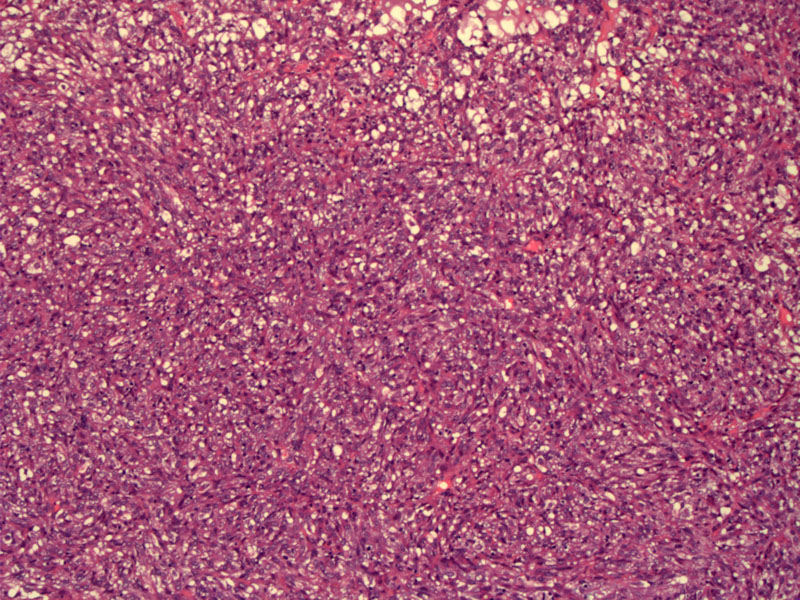
A low power, there is a proliferation of poorly-differentiated stromal cells.
The nuclei are pleomorphic and do not bear any resemblance to endometrial stromal cells in the proliferative phase. There are some ill-defined glands containing eosinophilic secretions.
A sheet of undifferentiated, atypical stromal cells is seen. These tumors are frequently mitotically active. Although not demonstrated here, foci of necrosis are commonly seen.
Historically, endometrial stromal tumors were divided into 3 categories: benign endometrial stromal tumors, low-grade endometrial stromal sarcomas and high-grade endometrial stromal sarcomas. One of the main features used to distinguish between low-grade and high-grade sarcomas was mitotic activity. However, it has since been established that mitotic activity has no prognostic value in these tumors.
Under the current WHO classification, low-grade endometrial stromal sarcoma encompasses all tumors composed of neoplastic proliferative-phase stromal cells regardless of mitotic activity. Tumors with pleomorphic stromal cells that did NOT resemble proliferative-phase endometrial stromal cells are designated as undifferentiated endometrial sarcomas (UES). The qualifier 'low-grade' is sometimes kept to avoid confusion with undifferentiated endometrial sarcomas, previously labeled high-grade endometrial sarcomas. However, the correct updated terminology is simply endometrial stroma sarcoma (ESS), as the distinction between high-grade and low-grade is no longer made.
Most authorities no longer consider UES as part of the endometrial stromal tumor family (now with two members, endometrial stromal nodule and endometrial stromal sarcoma). The tumor cells in UES bear little morphologic and immunohistochemical resemblance to endometrial stromal cells. Features seen in UES include high mitotic activity, marked cytologic atypia, loss of progesterone receptors and frequent necrosis.
These tumors typically occur in older women (compared to endometrial stromal tumors) and have a significantly worse prognosis.4
A recent study of 19 ESS and UES tumors demonstrated a 5 year survival rate of 91% for ESS and 33% for UES.4
• Myometrium : Leiomyoma, Highly Cellular
• Myometrium : Endometrial Stromal Sarcoma, Low-Grade
1 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 305.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 667-9.
3 Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2497-2501.
4 Bartosch C, Exposito M, Lopes JM. Low-Grade Endometrial Stromal Sarcoma and Undifferentiated Endometrial Sarcoma: A Comparative Analysis Emphasizing the Importance of Distinguishing Between These Two Groups. Int J Surg Pathol. 2009 May 29. [Epub ahead of print].