
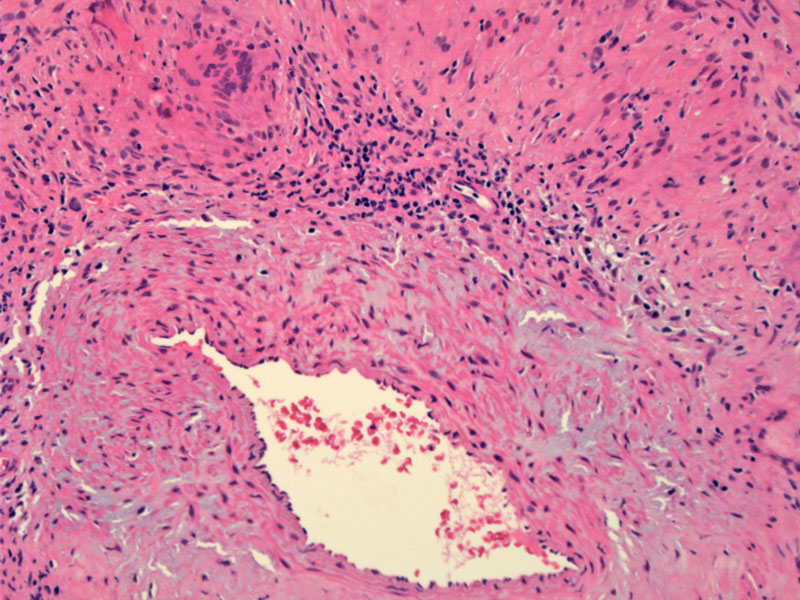
Giant cell arteritis is characterized by granulomatous inflammation of the media of medium to large arterities. Note the lymphocytes admixed with giant cells in the vessel wall and thickening of the intimal layer.
There is concentric involvement by inflammatory process, which narrows the lumen. This inflammation can lead to luminal occlusion, thrombosis and ischemia (Chew).
Several closely related multinucleated giant cells can be appreciated here.
Giant cell arteritis (GCA) is an autoimmune vasculitis which targets predominantly medium-sized to large arteries. Inflammation within the affected vessels leads to thrombosis and ischemia, causing the end organ manifestations of the disease. Most commonly the disease affects the head and neck including the vascular supply to cranial nerves, muscles of mastication, and intracranial circulation. Severe cases can manifest outside of the head and neck and include larger vessels such as the aorta (giant cell aortitis) and subclavian arteries. Vision loss resulting from of arteritic anterior ischemic optic neuropathy (AAION) is one of the most feared complications of this disease. Roughly 50% of patients will have visual axis involvement (Hayreh).
Temporal artery biopsy has been the mainstay of diagnosis, with other tests such as ESR and CRP being important for diagnosis and judging response to treatment. Due to the segmental nature of the lesion, multiple biopsies along at least 2-3 cm of the artery is recommended for adequate sampling (Kumar).
Histologically, the intimal layer is thickened. There is granulomatous inflammation consisting of mononuclear cells and giant cells in the inner (luminal) portion of medial layer, leading to destruction of the internal elastic membrane.
The presence of three or more of the following criteria is required for the diagnosis of giant cell arteritis:
- Age of onset greater than 50 years
- Onset of new headache
- Temporal artery abnormality (tender or reduced pulsation)
- Elevated erythrocyte sedimentation rate, defined as 50 mm/h using the Westergren method
- Abnormal arterial biopsy – showing necrotizing vasculitis with predominant mononuclear cell infiltration or granulomatous inflammation
GCA is usually seen in Caucasians and is in fact, the most common type of vasculitis in North America and Europe in individuals older than 70 (Gonzalez-Gay). Other common symptoms include scalp tenderness, jaw claudication as well as nonspecific constitutional symptoms such as fatigue, myalgias and weight loss. There is often an association with polymyalgia rheumatica. On physical examination, the temporal artery will be tender, with nodular thickenings (Kumar).
High-dose systemic corticosteroids are the mainstay of treatment. During exacerbations or at new diagnosis, improvement in symptoms is typically seen within 72 hours. Most patients continue oral prednisone for several weeks, tapering based on symptoms and serial monitoring of inflammatory markers. Here again, most patients will require treatment for a minimum of one to two years (Proven).
Relapses are typically associated with a recurrence of symptoms or a rise in ESR/CRP. and are more commonly seen in individuals with severe symptoms at presentation or a poor initial response to steroids.
Causes of mortality associated with GCA include cardiovascular, neurological and gastrointestinal events. Vasculitis of the coronary arteries may result in MI or CHF. Ischemic brain damage is the second most common cause of GCA-related death after cardiac disease, and occurs by either inflammatory obstruction of the vertebrobasilar or carotid arterial systems, embolism or propagation of thrombus from inflamed arteries to uninflamed arteries.
The prognosis for visual recovery is poor for individual with visual loss related to GCA, and continued visual deterioration occurs in about 25% of eyes despite high-dose intravenous steroids.
Chew SS, Kerr NM, Danesh-Meyer HV. Giant cell arteritis. J Clin Neurosci. 2009 Oct;16(10):1263-8. Epub 2009 Jul 7.
Gonzalez-Gay MA, Vazquez-Rodriguez TR, Lopez-Diaz MJ et al. Epidemiology of giant cell arteritis and polymyalgia rheumatica. Arthritis Rheum. 2009 Oct 15;61(10):1454-61.
Hayreh SS, Podhajsky PA, Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol 125 (1998), pp. 509–520.
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 537-8.
Proven A, Gabriel SE, Orces C et al. Glucocorticoid therapy in giant cell arteritis: duration and adverse outcomes. Arthritis Rheum 49 (2003), pp. 703–708.
Written by Garth Olson, M.D., Dept of Surgery, University of New Mexico.