
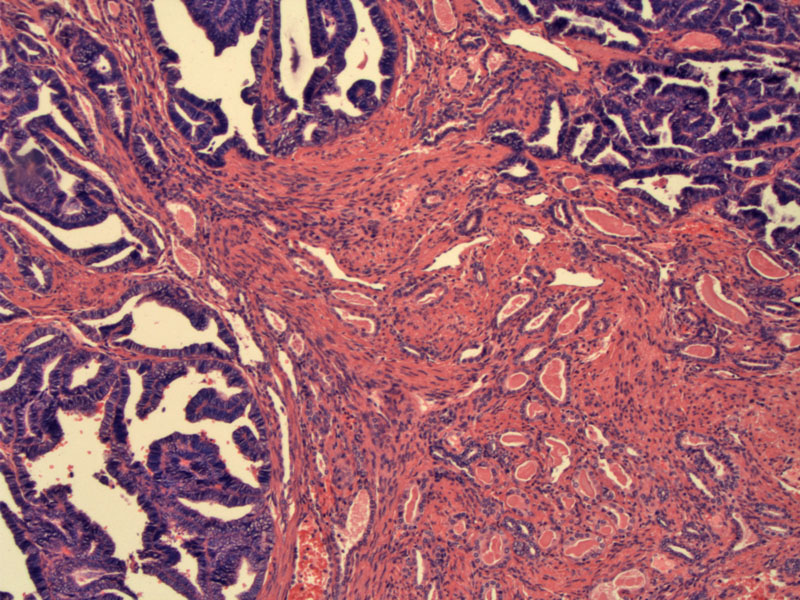
Case 1: A mixture of histological patterns is often seen. For example, this case demonstrates a ductal pattern consisting of darkly staining endometrioid-like glands adjacent to a tubular proliferation of malignant glands. The two patterns have strikingly different morphologies.
The tubules may be compressed, forming long cord-like structures. Note the adjacent endometrioid glandular structures in the upper left.
The tubular proliferation may resemble mesonephric hyperplasia and in fact, foci of mesonephric hyperplasia are usually present. Both consist of variably-sized tubules containing eosinophilic secretions.
A closer look at the endometrioid glands reveal crowded glandular structures with enlarged nuclei, mimicking endometrioid adenocarcinoma. However, in the latter, the nuclear atypia tends to be higher grade.
Case 2: This is a 47 woman who presents with a 10 cm mass in her cervix.
These glands involve most of the cervix. Areas of mesonephric hyperplasia could be found adjacent to the invasive component.
A higher power image demonstrates rather bland cytologic features.
CD10 demonstrates luminal positivity. CD10 is a helpful marker for cells of mesonephric origin, but not an entirely specific marker.
Calretinin was negative. This marker can be negative in 1/3 of cases and in this instance, the neoplastic glands did not stain (McCluggage).
ER was negative (seen here) as well as PR. This helps exclude endometrioid adenocarcinoma of the cervix or endometrium.
Mesonephric adenocarcinomas are derived from mesonephric remnants, vestigial structures of Wolffian ducts which form essential reproductive structures in men (efferent ducts, epididymis, vas deferens, seminal vesicles and ejaculatory ducts), but largely regress in women. Remnants of these ducts may persist in the broad ligament, vagina and cervix.
Mesonephric adenocarcinomas exhibit a broad range of architectural patterns. The two most common are ductal (resembling endometrioid adenocarcinoma) and tubular (resembling mesonephric hyperplasia). Other patterns include retiform (net-like), solid and spindled patterns. The spindled-pattern often appears biphasic, with the spindled component blending with the glandular component and some authors propose the term 'malignant mixed mesonephric tumor' to describe this variant.
Mesonephric hyperplasia vs mesonephric adenoma: Mesonephric adenocarcinoma should exhibit back-to-back glandular crowding, infiltrative glands and nuclear atypia. In contrast, mesonephric hyperplasia has a lobular configuration of tubules without cytologic atypia. In our particular case, the tubules are lined with bland cuboidal cells without cytologic atypia, however, the glands are starting to become quite crowded. Adjacent areas of mesonephric hyperplasia are often found in the majority of mesonephric adenocarcinomas.
In a study of 11 mesonephric adenocarcinomas, all were immunoreactive for epithelial markers such as AE1/3; CK1, CAM 5.2, cytokeratin 7, and epithelial membrane antigen. Most were positive for calretinin (88%), vimentin (70%), androgen receptor (33%), and inhibin (30%, focal staining). None stained with cytokeratin 20, estrogen receptor, progesterone receptor, and monoclonal carcinoembryonic antigen. This immunoprofile corresponds to that of mesonephric remnants and can help in differentiating between mesonephric adenocarcinoma from mullerian endometrioid adenocarcinoma (Silver).
Occurs over a wide age range (34-73). Commonly presents as abnormal vaginal bleeding. Very frequently, a mass (exophytic, polypoid, nodular and/or ulcerated) is detected. There can also be a diffuse enlargement of the cervix, so-called barrel cervix (Fletcher).
Mesonephric adenocarcinoma is very rare, therefore, large studies have not been possible. Straightforward conclusions cannot be drawn at this time. However, it appears that stage is an important prognostic factor. In a 2001 study of 11 mesonephric adenocarcinomas, 8 tumors were at stage IB. The two patients with advanced stages (IIB and IVB) had local recurrences and died at 3.2 and 0.8 years from the time of diagnosis. One case was not staged. Of the 8 patients with stage IIB, 6 remained alive without recurrence after 4.8 years (Silver).
Another study of 9 mesonephric adenocarcionmas demonstrated that a prominent spindled component (malignant mixed mesonephric tumors) may also connote a poorer prognosis as these tumors tend to present at a later stage and behave more aggressively, similar to mixed malignant mixed müllerian tumors (Bague).
→It is important to recognize this rare entity as can mimic either well-differentiated adenocarcinoma of the cervix OR endometrioid adenocarcinoma (of the endometrium) involving the cervix.
→In mesonephric adenocarcinoma, there ought to be foci of mesonephric hyperplasia containing eosinophilic secretions, a helpful diagnostic clue.
• Ovary : Mesonephric Adenocarcinoma from Cervix
Bagué S, Rodríguez IM, Prat J. Malignant mesonephric tumors of the female genital tract: a clinicopathologic study of 9 cases. Am J Surg Pathol. 2004 May;28(5):601-7.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 284-6.
McCluggage WG, et al. CD10 and calretinin staining of endocervical glandular lesions, endocervical stroma and endometrioid adenocarcinomas of the uterine corpus: CD10 positivity is characteristic of, but not specific for, mesonephric lesions and is not specific for endometrial stroma. Histopathology. 2003 Aug;43(2):144-50.
Silver SA, Devouassoux-Shisheboran M, Mezzetti TP et al. Mesonephric adenocarcinomas of the uterine cervix: a study of 11 cases with immunohistochemical findings. Am J Surg Pathol. 2001 Mar;25(3):379-87.
Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2420-2.
***Images courtesy of Dr. Lida Crooks, VAMC Albuquerque NM.