
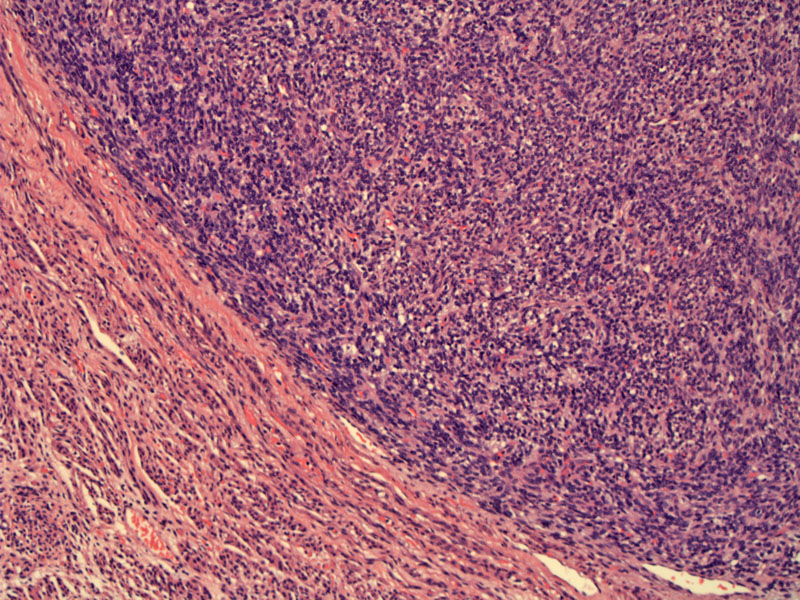
A sharply demarcated tumor-myometrial interface is one of the two key features separating a benign endometrial stromal nodule from a low-grade endometrial stromal sarcoma. The other key feature is the lack of lymphovascular invasion.
The stromal tumor cells are reminiscent of the stroma in proliferative phase endometrium. There is a diffuse sheet of small blue cells with oval to slightly elongated nuclei and scant cytoplasm.
The swirling short fascicles of neoplastic cells can be appreciated here. Although not demonstrated here, the neoplastic stromal cells sometimes swirl around the small arterioles.
Endometrial stromal tumors can be divided into three categories: (1) benign endometrial stromal nodules (2) low-grade endometrial stromal sarcoma and (2) undifferentiated (high-grade) endometrial sarcoma. The composite tumor cells are derived from the stromal component of endometrium and are the second most common mesenchymal tumor the uterus.
Benign stromal tumors are discrete well-circumscribed nodules that have a discrete interface between the neoplasm and surrounding myometrium. This is an important distinguishing feature between benign stromal tumors and low-grade endometrial stromal sarcomas. Slight focal interdigitation may be focally present in a benign nodule, but must not exceed 3 mm in depth.1,2 The lack of lymphovascular invasion is the other important distinguish feature, absent in benign stromal tumors and present in low-grade endometrial stromal sarcomas.
Previously, mitotic rates was an important feature in separating benign, low-grade and high-grade (undifferentiated) tumors, however, recent studies have show that mitotic activity has little prognostic value and thus, is no longer used as a stratifier. Furthermore, undifferentiated endometrial sarcoma (formerly high-grade endometrial stromal sarcoma) is no longer considered part of the endometrial stromal family group as these tumors do not show any histologic resemblance to endometrial stroma and antigenic studies have confirmed their unrelatedness.1
Mean age of diagnosis is 47; approximately 1/3 of cases are found in postmenopausal women. Presents with abdominal or pelvic pain +/- abnormal uterine bleeding.2
Grossly, these tumors can be polypoid (if located in the endometrium), or can be intramyometrial or subserosal nodules ranging from 0.5 to 22 cm (mean size of 7 cm). They have a soft, tan to yellow cut surface. Secondary cystic formation, hemorrhage or necrosis may occasionally be present.2
Excellent; complete excision is curative. Often, a hysterectomy is performed, however, excision of the tumor only is also acceptable if clear margins can be obtained.
• Myometrium : Endometrial Stromal Sarcoma, Low-Grade
• Myometrium : Leiomyoma, Highly Cellular
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 667-9.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 293-302.
3 Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2497-2501.