
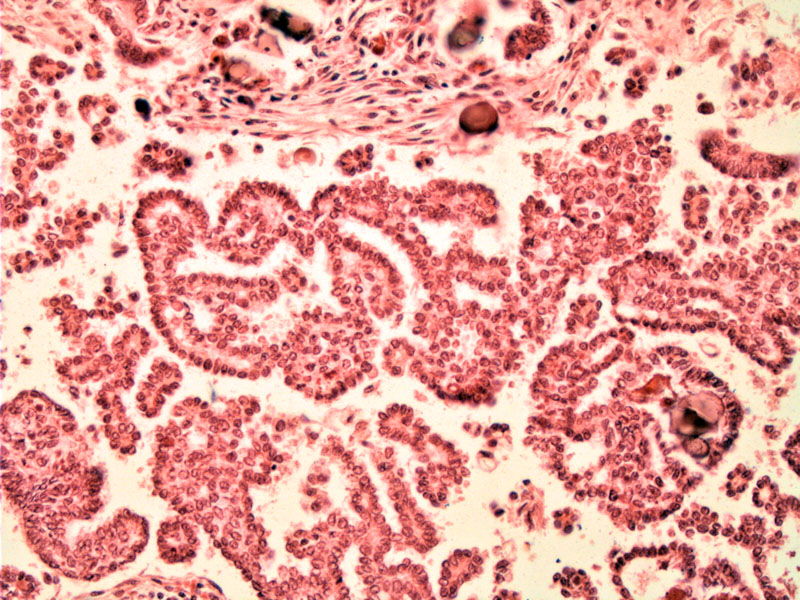
In this case of low grade serous carcinoma, papillary formations, psammomatous calcifications can be appreciated. Note that there is no signficant cytologic atypia.
In other areas of the tumor, clusters of malignant cells dissect into stroma (upper part)-- one can appreciate dense aggregates of small micropapillae resembling invasive micropapillary carcinoma of the breast and irregular infiltration of stroma by these cytologically malignant papillae.
Most cases of serous carcinoma are high-grade, however, a minority of cases are low-grade. There is no standardized grading scheme, however, many pathologists accept the Silverberg system which assigns a grade based on nuclear atypia, mitotic activity and architectural features. It is thought that most low-grade serous carcinomas arise from the progression of borderline serous tumors.1,2
Low-grade serous carcinoma vs borderline serous tumor with microinvasion:
The distinction of serous tumors of low malignant potential (S-LMP) (borderline tumors) from ovarian serous carcinoma relies on the absence of infiltrative destructive growth or obvious stromal invasion. We recognize that on occasion, the distinction between low-grade serous carcinoma and S-LMP can be quite problematic, especially in S-LMP with stromal microinvasion.
Clarification is helped by Bell and Scully who provided formal quantitative criteria for the diagnosis of stromal microinvasion (Bell 1990). Quantitative criteria specified no focus of microinvasion should measure 3 mm or more in greatest dimension, although some authorities have suggested a 5 mm maximum linear dimension. To account for the 3-dimensionality of these aggregates, this criterion was recently changed to a maximum area of 10 mm2 (Scully). If multiple foci are identified, it is recommended that the dimensions of these individual foci not be added together. As of yet, no study exist to provide sufficient outcome data to support or refute any of these various definitions.
A 2006 review by McKenney and colleagues seeks to further elucidate the significant of S-LMP with stromal microinvasion. Having examined 60 S-LMP with 'non-destructive' forms of microinvasion, they concluded that (1) microinvasion does indicate higher risk of disease progression; (2) microinvasion is more frequently found in pregnant patients although it does not appear to affect outcome in this group; (3) the micropapillary form of microinvasion may represent a higher risk lesion and should be duly noted on the pathology report (McKenney).
♣ Grading serous carcinomas is currently based on three features: nuclear atypia, mitotic activity and architectural features.
♣ Distinguishing between low grade serous adenocarcinoma of the ovary and serous tumor of low malignant potential (S-LMP) with microinvasion can be problematic.
♣ Microinvasion is currently quantified as less than 10 mm2 in area in area -- these serous tumors are still classified as borderline serous tumors with microinvasion. Invasion beyond this is classified as serous carcinoma.
• Ovary : Serous Cystadenofibroma
• Ovary : Serous Borderline Tumor
• Ovary : Serous Borderline Tumor, Micropapillary Type
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 574.
Bell DA, Scully RE. Ovarian serous borderline tumors with stromal microinvasion: a report of 21 cases. Hum Pathol. 1990;21:397–403.
McKenney JK, Balzer BL, Longacre TA. Patterns of stromal invasion in ovarian serous tumors of low malignant potential (borderline tumors): a reevaluation of the concept of stromal microinvasion. Am J Surg Pathol 2006 Oct;30(10):1209-21.
Scully RE, Young RH, Clement PB. Atlas of Tumor Pathology. Tumors of the Ovary, Maldeveloped Gonads, Fallopian Tube, and Broad Ligament. 3rd ed. Washington, DC: AFIP; 1998.