
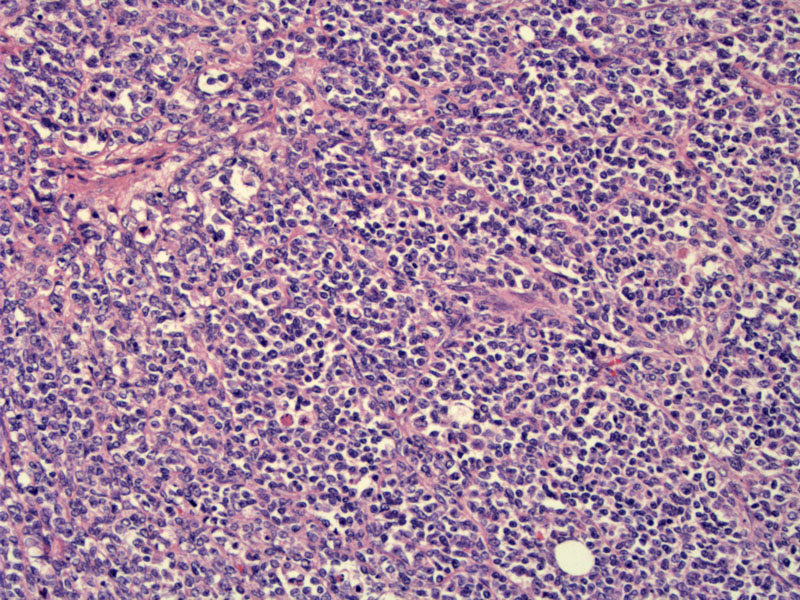
Monotonous small round cells with hyperchromatic nuclei and scant cytoplasm grow in diffuse sheets. Follicle-like spaces containing eosinophilic fluid may be seen in many cases.
There are two types of small cell carcinoma in the ovary:
(1) ovarian small cell tumor of the pulmonary type: this tumor is identical to small cell carcinoma arising from the lung. However, in this case, it arise from the ovary. This tumor is vanishingly rare and in fact, only a case series of 11 tumors has been reported and scattered single reports in the literature. The patient age ranges from 28 to 85 (mean of 59). The tumors may be either unilateral or bilateral. The prognosis is very poor, and in the case series of 11, 5 of 7 patients who had long-term followup did not survive beyond 13 months.1
Microscopically, small cells with scant cytoplasm, dark nuclei with granular chromatin which exhibit nuclear molding. Most of the tumors are associated with a surface epithelial tumor (either an endometrioid, mucinous, or Brenner tumor). These tumors must be distinguished from metastatic small cell carcinoma of the lung. TTF-1 has been proposed to separate the two (expected to be positive in lung primary and negative in ovarian primary), however, non-pulmonary small cell carcinomas may express TTF-1 and in reality, ovarian small cell tumors of the pulmonary type are so rare that an accurate immmunophenotype has not been described.1,2
(2) ovarian tumor of the hypercalcemic type: These neoplasms generally occur in young women and strongly associated with hypercalcemia. Most tumors are unilateral. Microscopically, a monotonous small round cells with scant cytoplasm grow in diffuse sheets and occasionally form trabecuale and cords. The nucleoli are generally inconspicuous. Follicular structures containing eosinophilic material are highly characteristic and are seen in 80% of the tumors. Mitotic figures are easily identified (usually exceed 20 MF per 10 HPF).
In 50% of cases, larger tumor cells with moderate to abundant cytoplasm are seen focally. If the large cells comprise a majority of the tumor, the tumor is designated as a 'large cell variant'. IHC studies demonstrate focal positive staining for EMA, cytokeratins, p53 and CD10 and diffuse reactivity for WT1 and calretinin. A few tumors are focally positive for neuroendocrine markers.1,2
Helpful features to distinguish between small cell carcinoma of the pulmonary type and small cell carcionma of the hypercalcemic type include: (1) the hypercalcemic type affects younger patients and is usually associated with hypercalcemia; (2) the pulmonary type is more often bilateral; (3) follicle-type spaces are highly characterisitc of the hypercalcemic type and nuclear molding is more typical of the pulmonary type; (4) an associated component of surface epithelial tumor favors the pulmonary type; (5) flow cytometry reveals the the hypercalcemic type is usually diploid, whereas the pulmonary type is usually aneuploid.1
Small cell carcinoma of the hypercalcemic type affects younger women (peak incidence in the late 20s and 30s) and two-thirds of cases are associated with hypercalcemia. Presentation is usually nonspecific and includes abdominal pain, nausea and vomiting. The hypercalcemia is usually asymptomatic.
Bilateral salpingo-oophorectomy and hysterectomy is recommended. The role of adjuvant therapy (chemotherapy and radiation) is unclear.
Prognosis is generally very poor and most cases present at an advanced stage. These are aggressive tumors with a high mortality rate. Stage is an important prognostic factor. In a series of 150 cases, 33% patients with stage IA tumors were alive with no evidence of disease at last follow-up, compared with 10% survival in stage IC tumors.2
• Endometrium : Small Cell Carcinoma
• Bladder : Small Cell Carcinoma
• Cervix : Small Cell Neuroendocrine Carcinoma
1 McCluggage WG. Ovarian Neoplasms Composed of Small Round Cells: A Review. Adv Anat Pathol 2004;11:288-296.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 587-8, 616-7.