
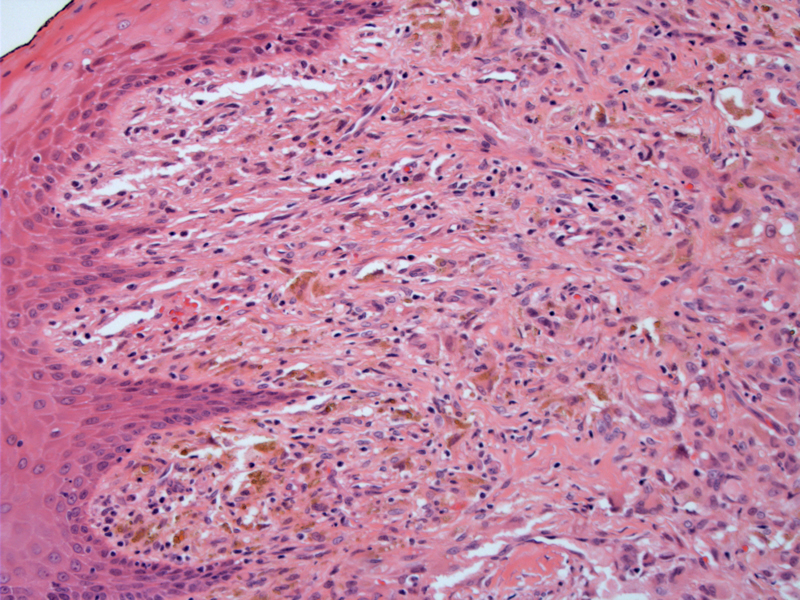
A superficial lesion consisting of a cellular infiltrate blends into overlying epidermis. However, the lesion does not involve the epidermis. Pigment incontinence and a giant cells (lower right) are seen.
The small- to intermediate-sized mononuclear histiocytes show a compact sheet-like infiltrate. Nuclei are small, round to ovoid and the cytoplasmic borders are indistinct. The lipid content of the histiocytes can vary, with early lesions demonstrating less lipid or
Scattered inflammatory cells consisting of lymphocytes and eosinophils (although mainly lymphocytes are seen here) and occasional mitotic figures may be encountered as a normal part of JXG. Note the foamy and vacuolated cytoplasm of the histiocytes.
Multinucleated giant cells with a so-called Touton configuration (wreath of nuclei) are characteristic of JXG. However, these giant cells may be focal in distribution and their detection is not a requirement for the diagnosis.
Histiocytosis is a broad term to describe proliferative disorders of dendritic cells and macrophages. A subset of these entities involve the proliferation of an immature dendritic called the Langerhans cell (with their trademark Birbeck granules), and thus are called Langerhans cell histiocytosis or the older obsolete term histiocytosis X. Juvenile xanthogranuloma (JXG) is one of the most common non-Langerhans histiocytic disorders that occurs in childhood.
JXG is divided into infantile (more common) and adolescent/adult types.1
- In the infantile type, the nodular lesions are located primarily in head, followed by trunk and extremities. The lesions are more likely than adolescent/adult types to be multifocal and usually spontaneously involute. 70% are diagnosed by age 1, and 20% are congenital. 5% occur in extracutaneous sites such as mucosal surfaces, viscera, skeletal muscle and CNS. Of the extracutenaous sites, the eye is most common.
- In the adolescent/adult type, the peak incidence in the 2nd to 3rd decades of life, and the lesions are generally solitary and found on the head. Truncal and extremity lesions are rare. Unlike infantile lesions, recurrence after excision is common and do not spontaneously involute. Extracutaneous involvement is uncommon, although several cases of ocular and systemic involvement of JXG in adults have been reported in the literature.
JXG is associated with neurofibromatosis type I and juvenile chronic myelogenous leukemia. Although the underlying pathogenesis is not well understood, a patient with JXG and NFI is 32 times more likely to develop juvenile CML (Putnam)
Microscopically, JXG has been divided into three patterns according to the age of the lesion (Putnam).
- Early or xanthomatous phase: Uniform proliferation of histiocytes with varying lipid content. Mitotic activity can be seen. Inflammatory cells are few and giant cells are located in the deep portion of the lesion (superficial biopsies may miss them).
- Classic or mature phase: Infiltrate of foamy, lipid-laden histiocytes admixed with Touton giant cells. Inflammatory cells, namely lymphocytes and eosinophils, are more prominent.
- Late phase: Also known as the transitional or fibrohistiocytic JXG, a spindled fibroblastic population is prominent thus, giving an overall picture of fibrosis.
Basically, early lesions may not contain the telltale giant cells or foamy histiocytes, so called "non-lipidized JXG". However, as the lesion matures, Touton giant cells and foamy histiocytes are readily seen. As the lesion ages or regresses, fibrosis sets in. Note that all three patterns can be seen in the same lesion.
IHC will be helpful in distinguishing JXG from other entities on the differential. For example, JXG is CD68, HAM56 (macrophages) and Factor 13a positive (dermal dendrocytes). Langerhans cell histiocytosis is S100 and CD1a positive, and these two markers are negative in JXG. Melanocytic nevi will stain positively with melanocytic markers such as S100, HMB45 and would be negative for CD68, Factor 13a and CD1a.
The majority of affected patients are infants and young children, although JXG can be seen in adults. There is a slight male predilection (M:F ratio of 1.5:1). Clinically, the soft yellow-orange-brown nodules are small (0.1 to 1.0 cm in diameter) and located on the head, followed by the trunk and extremities. The lesions are usually solitary (but may be multiple especially in younger patients).
Generally excellent as the lesion is benign. However, ocular complications can occur if lesions occur in the eye. For example, involvement of the iris can lead to uncontrolled glaucoma and blindness. Systemic juvenile xanthogranuloma is a very rare form which can be fatal if the CNS or viscera is extensively involved.
→Multiple JXG lesions and cafe au lait spots may indicate NF1, the combination of NF1 and JFG carries a 20x increased risk for developing childhood chronic myelogenous leukemia (Rapini).
→Histologically, in younger lesions, there are lymphocytes, histiocytes, and eosinphils, whereas in older lesions, foamy histiocytes and Touton giant cells are prominent.
→The histiocytes would be positive for CD68, HAM56 and factor 13a. They would be negative for S100 and CD1a (which are positive in Langerhans cell histiocytosis).
Janssen D, Harms D. Juvenile xanthogranuloma in childhood and adolescence: a clinicopathologic study of 129 patients from the kiel pediatric tumor registry. Am J Surg Pathol. 2005 Jan;29(1):21-8.
Putnam A, Lowichik A, Coffin CM et al. Juvenile Xanthogranuloma. Pathology Case Reviews. 2009;14: 104-109.
Rapini RP. Practical Dermatopathology. Philadelphia, PA: Elsevier; 2005: 110-1.