
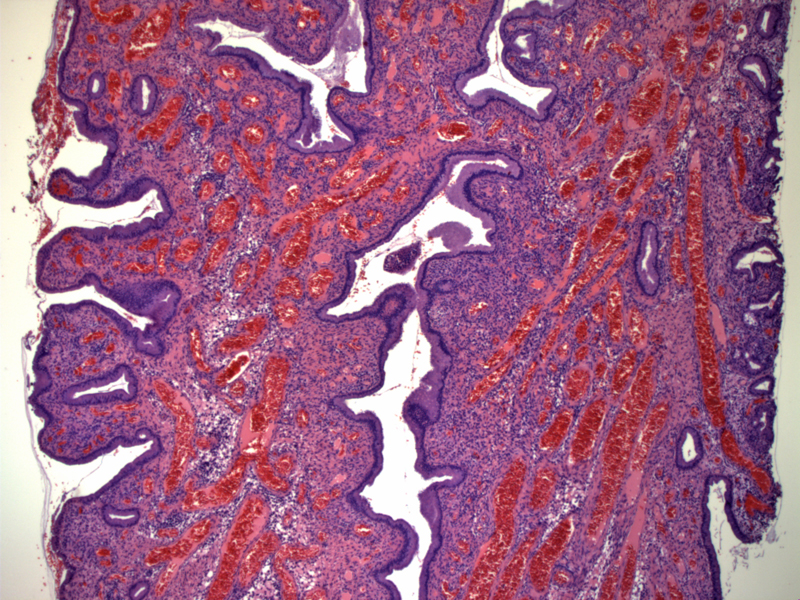
This typical endocervical polyp exhibits a polypoid structure with an even mixture of glandular and stromal components. It is covered by endocervical glandular epithelium. Endocervical polyps with microglandular hyperplasia would have much more prominent infoldings and undulations of the epithelium. A stromal-predominant polyp would consist mainly of stroma with a few glands.
Not uncommonly, the polyp may be very vascular with a proliferation of ectatic vessels. Clinically, this would be seen as a reddened polyp. A chronic inflammatory infiltrate is usually seen in the stroma.
A different polyp exhibits microglandular changes along the surface. Note the infoldings and undulations of the surface epithelium. Due to the tangential cut of the section, many tubular glands appear to lie within the stroma. There will be some glands within the stroma not continuous with the surface epithelium.
This endocervical polyp has a prominent stromal component. Not infrequently, the surface may be inflamed. Note the dense infiltrate of lymphocytes toward the epithelial surface.
The endocervical polyp can have a prominent stromal component. The stromal cells may exhibit mild atypia.
Similar to endometrial polyps, thick-walled vessels may be seen.
Squamous metaplasia replaces some of the surface mucosa of this inflamed polyp
Endocervical polyps are composed of a mixture of glands and stroma. The histology can vary depending on the proportion of the two components. The "typical" endocervical polyp has a fairly even mixture of both glandular and stromal components. However, the polyp can have a predominant glandular component and display infoldings of the epithelium -- sometimes described as "microglandular changes" or "microglandular hyperplasia". The polyp can also be stromal predominant with few scatter atrophic glands.
When a polyp is very vascular, it may be called a "vascular polyp". Squamous metaplasia can frequently involve in the surface or glandular epithelium. Rarely, the polyps may exhibit glandular and stromal atypia, and thus, must be distinguished from well-differentiated low-grade adenosarcomas.
Occurs at a wide age range with a mean incidence in the 5th decade. The polyps average 1 cm in size, and most are located in the cervical os. Polyps higher up in the lower uterine segment may contain both endocervical and endometrial glands, thus are termed "mixed endocervical/endometrial" polyps.
A significant proportion of patients present with bleeding and mucoid discharge. Because most endocervical polyps occur in post-menopausal women, additional workup must be undertaken to exclude endometrial carcinoma.
Treatment is with polypectomy. As many endocervical polyps present with abnormal bleeding, a workup for abnormal bleeding should be performed including endometrial sampling in patients at risk for endometrial carcinoma.
While recurrence is possible, endocervical polyps that cause symptoms are very rare and most women will remain symptom free after polypectomy.
1 Crum CP, Lee KR. Diagnostic Gynecologic and Obstetric Pathology. Philadelphia, PA: Elsevier; 2006: 419-20.
2 Kurman,R. Ed. Blaustein's Pathology of the Female Genital Tract. 5th Ed. New York, NY: Springer-Verlag; 2002: 242-3.
3 Robboy SJ, Anderson MC, Russell P. Pathology of the Female Reproductive Tract. London, UK: Churchill Livingstone; 2002: 133.