
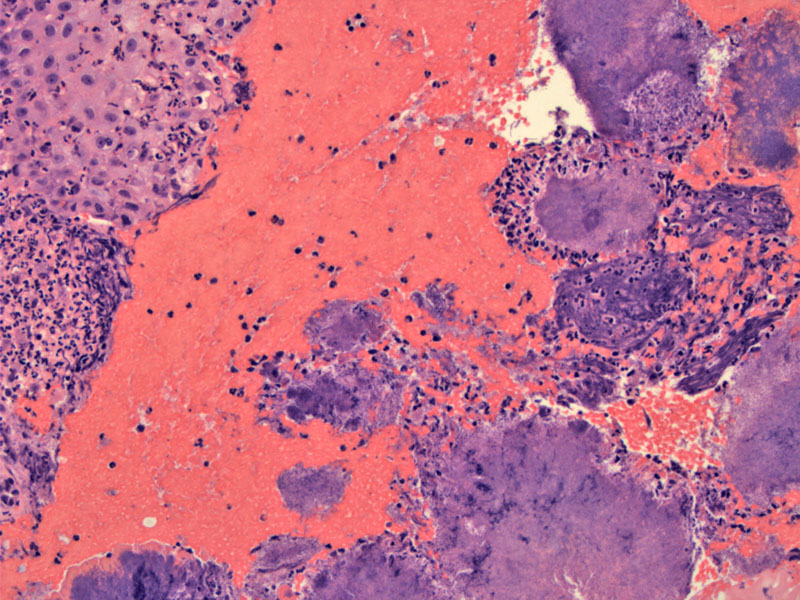
Sulfur granules (round filamentous colonies of A. israelii) are surrounded by inflammatory cells.
In a pap smear, Actinomyces colonies are seen as a sunburst colony with radiating filamentous organisms visible along the edge.
One of the more commonly isolated species in pelvic actinomycosis is Actinomyces israelii. Actinomyces are filamentous, non-acid-fast, non-spore-forming bacteria -- they are taxonomically close to hyphae bacteria, rather than fungi.
Actinomyces israelii can be found in up to 27% of asymptomatic women without an intrauterine device. Symptomatic cases tend to be seen in women with a foreign body in the uterus or vagina such as an IUD or less frequently, suture material. Symptomatic A. israelii infection is more common in those with plastic IUDs than with copper IUDs and in women who with an IUD for more than 4 years.1
Microscopically, the bacteria exist as a tangle of filaments or 'sulfur granules'
The inflammatory response is usually robust and consists of plasma cells, lymphocytes and neutrophils.
Symptoms include postcoital bleeding, vaginal discharge, pruritis or pelvic pain secondary to abscess formation.2
A search on current medical literature does not reveal a consensus paper on the treatment of actinomycosis in women with an IUD. Many women harboring A. israelii are asymptomatic. It is difficult to predict who will develop symptomatic pelvic inflammatory disease, which causes significant morbidity and may even be life-threatening.
Some authorities propose prophylactic treatment via changing of the IUD every four years and/or giving antibiotics if A. israelii is detected in a Pap smear.1 Other evidence suggests that a positive culture does not necessarily require the removal of an IUD and, in the absence of evidence for pelvic infection, antibiotics are not necessary.3
1 Evans DT. Actinomyces israelii in the female genital tract: a review. Genitourin Med. 1993 Feb;69(1):54-9.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 81-2, 344-6.
3 Lippes J. Pelvic actinomycosis: A review and preliminary look at prevalence. American Journal of Obstetrics and Gynecology. Volume 180, Issue 2, February 1999, Pages 265-269.