
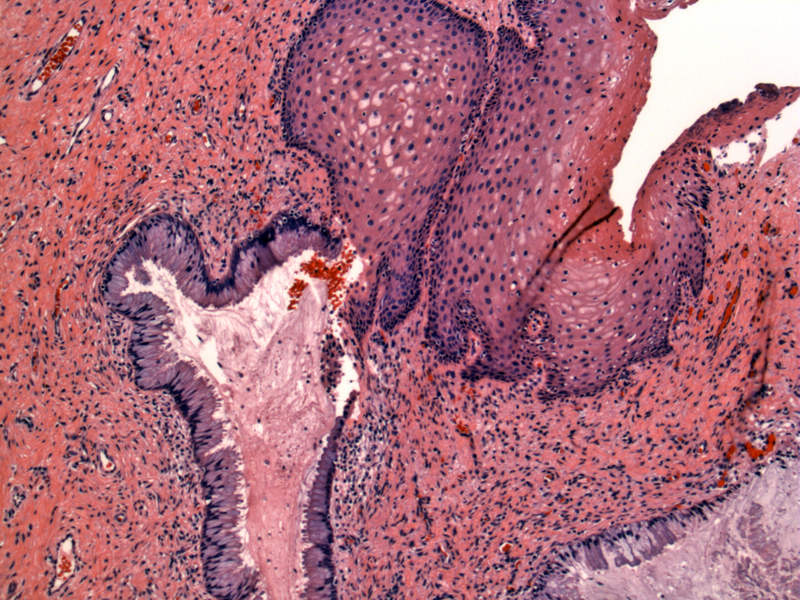
Emanating from normal squamous epithelium are benign glands lined by endocervical type cells (lower left). Endocervical glands can undergo squamous metaplasia as seen here. Eventually, the metaplastic squamous epithelium is replaced by mature glycogenated squamous epithelium.
Endocervical glands are seen in the lamina propria with an intact overlying epithelium.
Vaginal adenosis is most famously associated with in utero exposure to DES. The risk of developing adenosis depends on the the dose of DES administered and the gestational stage at exposure. For example, all women who were exposed to DES before the 8th week of gestation developed vaginal adenosis, however, only 6% of women exposed after the 15th week of gestation developed vaginal adenosis (Nucci, Sternberg).
Vaginal adenosis is the presence of endocervical or endometrial glandular epithelium within the vaginal wall. Remember that the vagina should be lined entirely by non-cornified squamous epithelium. The glandular epithelium can be continuous with the surface squamous epithelium, so called surface adenosis which imparts a red granularity on clinical examination or the glandular epithelium can form glands in the lamina propria with an overlying intact squamous epithelium, so called occult or cystic adenosis. These glands are thought to be persistent Müllerian columnar epithelium. DES prevents urogenital squamous epithelium from replacing this columnar epithelium during fetal development (Kranl).
As mentioned above, vaginal adenosis comes in two main variants: endocervical and tuboendometrial type. Tuboendometrial-type glands are rarer and may be the more direct precursor to clear cell adenocarcinoma. One study reported that 94% of invasive clear cell carcinoma had adjacent tuboendometrial-type glands (Sternberg). Tuboendometrial-type glands in the lamina propria may mimic endometriosis, however, there is no associated endometrial stroma.
It is important to remember that vaginal adenosis can develop from causes other than DES. Up to a third of women with vaginal adenosis do not have a history of DES exposure. Acquired vaginal adenosis can result from topical 5-fluorouracil therapy for condyloma acuminata or following vaginal epithelial trauma such as an episiotomy. Spontaneous vaginal adenosis also exists.
Mostly, vaginal adenosis is benign and needs no treatment other than close observation. Excision may be necessary for florid cases. A small percentage of women develop clear cell adenocarcinoma (1 in 1000 DES exposed women). The incidence of squamous intraepithelial neoplasia of vagina or cervix is also twice as high in DES-exposed women compared to non-exposed women (Sternberg).
→The vagina is normally lined by noncornified squamous epithelium. Vaginal adenosis is defined as endocervical or endometrial glands within the vaginal wall.
→Associated with DES exposure in utero.
→Slightly increased of transformation into clear cell adenocarcinoma of the vagina.
• Vagina : Clear Cell Adenocarcinoma
• Cervix : Clear Cell (Adeno)carcinoma
1 Sternberg SS, ed. Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: 2356-7.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 95-6.
3 Kranl C, Zelger B, Kofler H, et al. Vulval and vaginal adenosis. Br J Dermatol. 1998 Jul;139(1):128-31.