
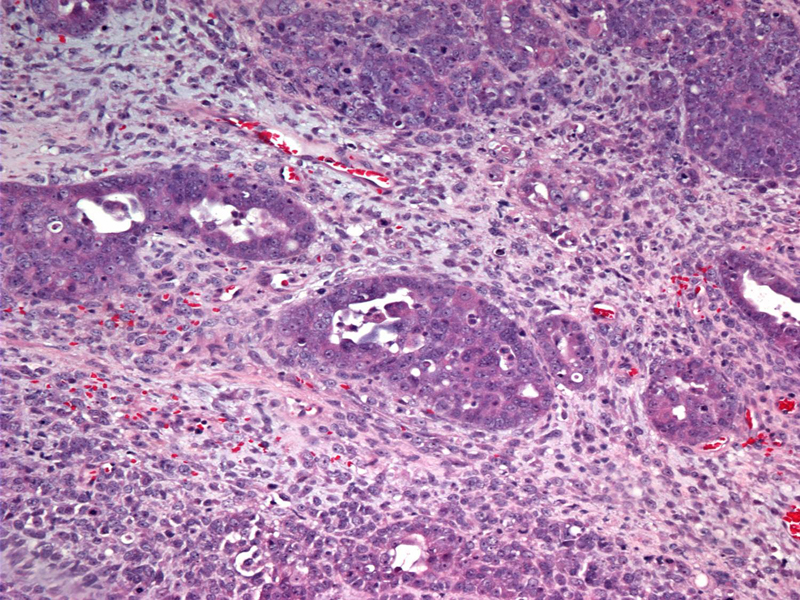
The malignant epithelial component is usually comprised of endometrial-type or serous-type adenocarcinoma. In this case, papillary serous type glands are surrounded primitive mesenchymal stroma.
In areas of this tumor, ill-defined malignant glands blend imperceptibly into malignant stromal elements.
FNA (Pap stain) of subsequent recurrent disease in the pelvis demonstrates loose clusters of malignant carcinomatous cells.
A closer look (Diff-Quik stain) reveals significant nuclear pleomorphism and prominent nucleoli. Note the wide range of sizes in the nuclei. The cytoplasm is stripped away in many of the cells.
A biopsy of recurrent disease reveals a diffuse sheet of malignant squamoid epithelial cells. Recurrent or metastatic disease in MMMT is often carcinomatous and not sarcomatous.
A different case demonstrates an undifferentiated carcinomatous component with extensive confluent (geographic) necrosis.
Undifferentiated blue cells comprises most of this tumor. The pale pink fibrous bundles is probably background ovarian stroma. The sarcomatous component of this tumor is difficult to distinguish and may not be present. Remember that MMMT is a metaplastic carcinoma and the sarcomatous component is most likely derived from the carcinomatous component. In this particular tumor, the sarcomatous component may not have differentiated from the carcinomatous component.
Yet another case demonstrates an admixture of carcinomatous and sarcomatous cell types.
At higher power, cells with bright pink cytoplasm, cells with hyperchromatic bizarre nuclei and nondescript cells with ovoid vesicular nuclei are blended together.
A closer look of the eosinophilic cells shows they have primitive rhabdomyosarcomatous appearance, thus, this tumor demonstrates heterologous mesenchymal elements. These rhabdomyosarcomatous cells mingle with bizarre hyperchromatic enlarged cells. The lower half of the image shows a less differentiated mesenchymal stroma.
Another area shows a haphazard distribution of malignant glands surrounded by malignant stromal cells.
An undifferentiated area composed of dark blue polygonal cells grow in broad anastamosing trabeculae. Note the high mitotic count.
Primitive mesenchymal malignant cells with scattered dark and highly atypical nuclei.
High grade epithelial adenocarcinomous component with a psammoma body (right of center) can be seen. This epithelial component resembling a high-grade papillary serous carcinoma merges with malignant stromal cells (upper right).
Malignant mixed mesodermal tumor (MMMT, carcinosarcoma) is the ovarian counterpart of malignant mixed mullerian tumor in the uterus. For some reason, the term mesodermal is more commonly applied to ovarian tumors, whereas the term mullerian is applied to uterine tumors. However, it is the same tumor in different locations of the female genital tract. MMMT is far more frequent in the uterus than in the ovary, and they can also (very rarely) occur in the cervix and fallopian tube.
In the ovary, MMMT is categorized under endometrioid epithelial tumors because they are virtually identical to MMMT of the endometrium. Microscopically, there is an intimate admixture of a malignant epithelial component and a malignant mesenchymal component. The epithelial component is usually an endometrioid or serous carcinoma -- although mucinous, clear cell, squamous and undifferentiated carcinomas may be seen. The mesenchymal element may be homologous (fibrosarcoma, leiomyosarcoma, endometrioid stromal sarcoma) or heterologous (rhabdomyosarcoma, chondrosarcoma, or osteosarcoma).
IHC and genetic studies have supported a clonal origin of this tumor, rather than a collision of two malignant elements. Specifically, the sarcomatous component is derived from the carcinomatous component, which arises from a stem cell. Thus, MMMT are best described as metaplastic carcinomas. Support for this theory includes: (1) the sarcomatous component exhibits epithelial markers; (2) the prognosis depends on the grade of the epithelial component whereas the histologic appearance of the sarcomatous component has little prognostic significance; (3) tumor emboli in the lymphatics, metastatic and recurrent tumors are usually carcinomatous rather then sarcomatous.1,2
Typically arise in elderly postmenopausal women. Recent studies have shown that risk factors for MMMT are similar to those of endometrioid (type I) endometrial adenocarcinomas. Both entities are associated with hyperestrogenism (obesity, nulliparity), and oral contraceptives are protective.3
Presents with abdominal pain and weight loss. Serum CA-125 is usually elevated. A palpable mass and ascites may be present on physical exam.
Surgical staging is as for epithelial ovarian cancers. As these are very rare tumors, adjuvant therapy is ill-defined.
MMMT are highly aggressive neoplasms that typically present at an advanced stage (FIGO III or IV). Prognosis is grim; in a study of 400 patients with MMMT, the median survival was 6-12 months and 70% were dead within one year.4
1 Mills SE, ed. Sternberg's Diagnostic Surgical Pathology.4th Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004: PAGE.
2 Costa MJ, Khan R, Judd R. Carcinoma (malignant mixed müllerian [mesodermal] tumor) of the uterus and ovary. Correlation of clinical, pathologic, and immunohistochemical features in 29 cases. Arch Pathol Lab Med 1991 Jun;115(6):583-90.
3 McCluggage WG. Malignant biphasic uterine tumours: carcinosarcomas or metaplastic carcinomas? Journal of Clinical Pathology 2002;55:321-325.
4 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 582-3.
Images from third case courtesy of Dr. Lida Crooks, VAMC Albuquerque New Mexico.