
A papillary adenoma (also known as renal cortical adenoma) is well-circumscribed but not encapsulated. Sometimes, there may be a fibrous pseudocapsule. The interface between the neoplasm and normal renal parenchyma lacks inflammation or a stromal reaction.
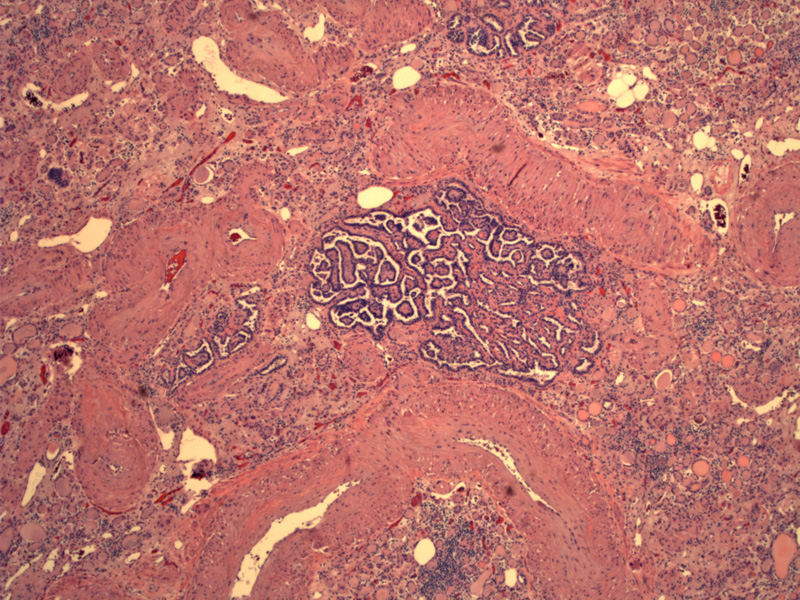
Another image demonstrates a small well-circumscribed papillary adenoma. The architecture is tubular, papillary or tubulopapillary. Note the fibrovascular core projecting into the lumen
Psammomma bodies are often present. This particular lesion demonstrates a tubulopapillary architecture.
In this case, the tubules are lined by monomorphic cells with round nuclei and scant pale cytoplasm. The cell types in a papillary adenoma generally resemble those in type 1 of papillary renal cell carcinomas, but rarely, one will find the pink abundant cytoplasm typical of type 2 papillary renal cell carcinomas.
The lining cells contain round nuclei with inconspicious or small nucleoli, similar to Fuhrman grade 1 or grade 2. There should NOT be prominent pleomorphism, and mitotic figures are largely absent.
Papillary adenomas, also known as renal cortical adenomas, are often incidental findings. The following criteria have been established and largely accepted for the diagnosis of papillary adenomas.1
- Papillary or tubolpapillary architecture
- Diameter less than 0.5 cm.
- Does not resemble clear cell, chromophobe, or collecting duct renal cell carcinomas
There has been debate regarding the possible malignant nature of these little neoplasms. Although papillary adenomas are deemed benign, some authorities say that the only truly benign renal epithelial neoplasms are oncocytomas and metanephric adenomas.2 Furthermore, as these lesions are morphologically identical to low-grade papillary renal cell carcinomas, and all neoplasms were small at some point in their development. However, if the patholology strictly adheres to the above criteria, these little papillary neoplasms do not exhibit malignant potential.
Autopsy studies have reported an incidence as high as 22% and appears to increase with age to 40% in those over 40.1,3
More frequently found in kidneys with chronic pyelonephritis, acquired renal cystic disease (from long-term dialysis) or renal vascular disease. They are also features of von Hippel-Lindau syndrome.1,2 Furthermore, kidneys with oncocytomas and renal cell carcinomas are more likely to contain papillary adenomas.
Grossly, the yellow-gray nodules are well-circumscribed but nonencapsulated. Most of solitary, but multiple nodules do occur and if extensive, the term "renal adenomatosis" is used.
Excellent; these tumors are benign.
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 485-6.
2 Zhou M, Magi-Galluzzi, C. Genitourinary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2006:300-1.
3 Murphy WM, Grignon DJ, Perlman EJ. Tumors of the Kidney, Bladder and Related Urinary Structures. AFIP Atlas of Tumor Pathology. Fourth series, Fascicle 1. Washington DC; AFIP: 2004; 160-4.