
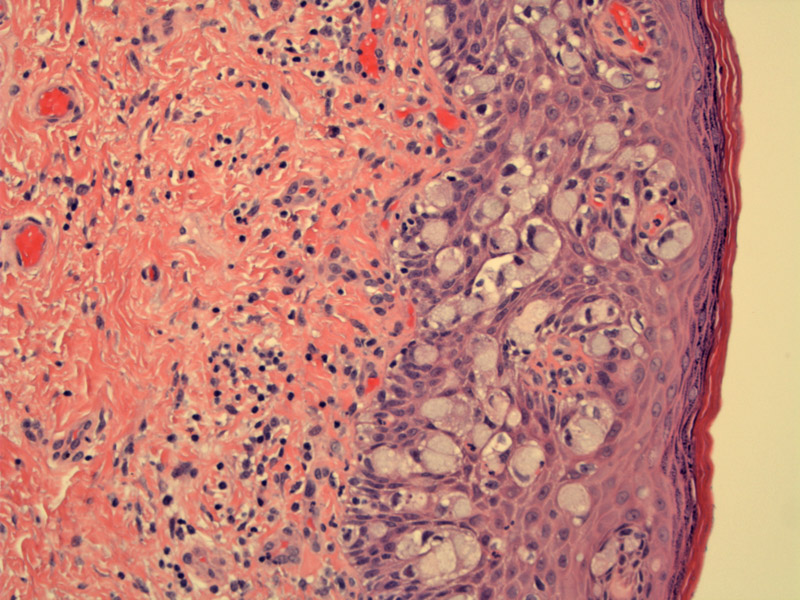
Case 1: The vulvar squamous epithlium contains large cells with pale blue cytoplasm consistent with extramammary Paget disease. The malignant glandular cells may originate from apocrine gland ducts or possibly from keratinocytic stem cells.
These large cells would be strongly positive for keratin 7 and CEA (supporting an adenocarcinoma).
Clinical Image: Erythematous lesion is fairly nonspecific and may be mistaken for a dermatitis.
Case 2: The inflammatory component partially obscures the malignant cells, making the diagnosis more challenging.
In such instances, immunohistochemistry for CK7 or CEA (shown here) is highly useful to identify the intraepithelial malignant cells.
The pattern of spread can mimic melanoma, therefore, one might consider melanocyte markers.
Extramammary Paget disease (EMPD) is clinically and histologically identical to mammary Paget disease of the nipple, however, important differences must be noted. Mammary Paget disease is the colonization of the epidermis by an underlying ductal carcinoma of the breast i.e. a secondary process.
EMPD does not arise in the breast, but in locations rich in apocrine glands such as the genital area and axilla. Furthermore, the majority of EMPD is a primary intraepidermal adenocarcinoma, that is, where the neoplastic glandular cells are posited to originate from intraepidermal apocrine ducts or possibly a pluripotent keratinocytic stem cell. The exact cell of origin is still unclear. Only ~25% are secondary processes (like mammary Paget disease), where there is an underlying adenocarcinoma from a deeper adnexal structure or an adenocarcinoma from Bartholin glands, urethra, bladder, vagina, cervix, endometrium, and prostate (Busam, Sandu, Lloyd). If the perianal region is the primary site, the risk of underlying colorectal carcinoma may be as high as 25-30%.
Although not common, EMPD must always be considered in patients with genital or perianal dermatitis.
Vulvar Paget disease may appear as a dermatitis (eczema, psoriasis), lichen sclerosis, thus, there may be a delay in biopsying and treating the lesion.
Key entities on the differential diagnosis include melanoma in situ (use melanocyte markers), and Bowen disease (positive for AE1:AE3). One must also look for secondary involvement from adjacent malignancies (secondary extramammary Paget disease). Most primary EMPD are CK7+/CK20- whereas EMPD secondary to a colorectal or urinary adenocarcinoma would be CK20+ (Busam).
Typically affects those in the 50-60 age range. Women are affected 4-5 times more often than men. Pruitis is usually the only presenting complaint. Classically the lesions are very erythematous and well demarcated. Over time the pruritis leads to excoriations and lichenification.
Because the disease usually extends beyond its visible margins, treatment includes wide and deep surgical resection comprising all the skin appendages. However there remains a high frequency of recurrences (15-62%), often irrespective for radicality of surgical excision (Preti). When associated with underlying invasive adenocarcinoma or stromal invasion, vulvar surgical approach must be integrated with inguino-femoral lymphadenectomy.
Recurrences or progression of intraepithelal vulvar Paget's are reported as far out as >10 years (average 2.5 years) from first surgical resection, necessitating long term follow-up (Preti).
→The majority of EMPD cases are primary intraepithelial adenocarcinomas. Only a subset are associated with an underlying malignancy. In contrast to mammary Paget disease where it is a secondary disease process (colonization of the epidermis by an underlying ductal carcinoma of the breast).
→The malignant glandular cells should be CEA positive, CK7 positive, GCDFP15 positive and express gastric mucins (MUC1+, MUC2-, MUCH5AC+).
Busam KJ. Dermatopathology: Foundations in Diagnostic Pathology 1st Ed. Philadelphia, PA: Elsevier; 2010: 422-4.
Lloyd J, Flanagan AM. Mammary and extramammary Paget's disease. J Clin Pathol. 2000 Oct;53(10):742-9.
Preti M, et al. [Vulvar Paget's disease. Clinico-pathologic review of the literature]Minerva Ginecol. 2000 May;52(5):203-11.
Sandu N. Extramammary Paget Disease: eMedicine. Last updated on Oct 20 2011. Available at: emedicine.medscape.com/article/1100397
Clinical image kindly contribued by Dr. Alan Waxman, UNM Dept of ObGYN, Albuquerque New Mexico.