
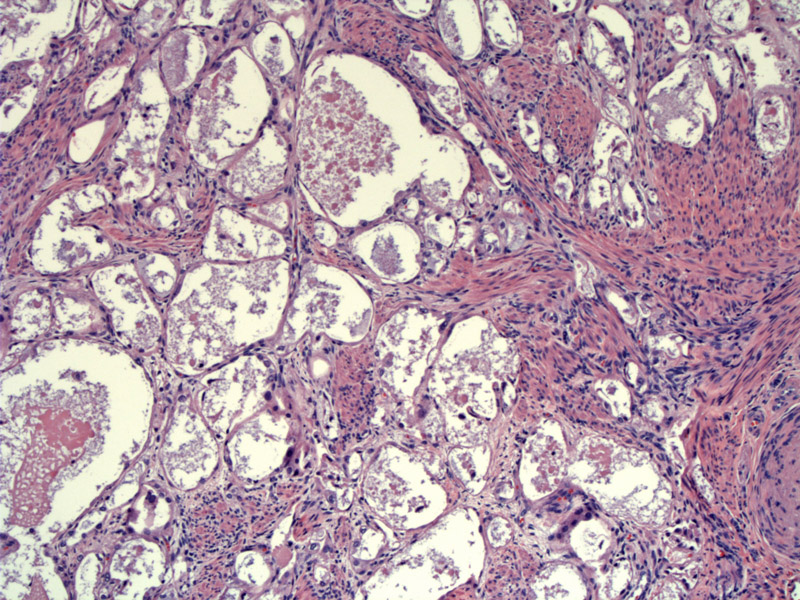
Clear cell adenocarcinoma of the cervix and vagina resembles clear cell carcinomas elsewhere in female genital with glycogen-rich tumor cells arranged in tubulocystic structures. Other common architectural patterns include solid or papillary growths.
Tumor cells lining the tubulocystic structures can be attenuated, with bland nuclei and scant cytoplasm. Note a few clear cells with abundant intracytoplasmic glycogen in the center of the image. Despite its name, clear cells do not usually make up the majority of the lesion. Hobnail cells are the most abundant cell types (as demonstrated in later images).
One will usually find areas containing cells with significant cytologic atypia. These tumor cells clearly exhibit hyperchromatic nuclei with irregular nuclear contours and size variation.
Another view of cystic structure lined by flat attenuated cells. The cystic glands in right upper corner are lined by cells with larger nuclei and more abundant cytoplasm. Some even have a hobnail appearance with nuclei protruding into the lumens.
A papillary configuration is often seen as well, lined by lesional cells with clear cell and hobnail cell morphology.
The tumor cells exhibit prominent nucleoli, irregularly contoured nuclei, and moderate pleomorphism.
Clear cell adenocarcinoma is most often seen in the vagina, however, they can also arise in the cervix (as in our case). These neoplasms may be sporadic or associated with in utero exposure to DES. Diethylstilbestrol or DES was prescribed for women during between 1940 to early 1970s for the prevention of miscarriages. This practice was stopped once DES was discovered to be a teratogen, however, approximately 2 million women in the United States were exposed to DES in utero.1
Aside from an increased risk of developing clear cell adenocarcionma of the vagina and cervix, DES also causes abnormalities such as cervical ectropion (when columnar epithelium protrudes through the external os), vaginal adenosis and cervical hypoplasia. Note that vaginal adenosis is found in the majority (>90%) of cases and is thought to be a precursor lesion to clear cell carcinoma.
The main differential diagnosis for clear cell carcinoma are two non-neoplastic entities that can occur in the cervix or endocervical-type glands formed in vaginal adenosis:
(1) microglandular hyperplasia - the proliferation of small glands lined with vacuolated cells may mimic clear cell carcinoma, especially since microglandular hyperplasia can also have a solid growth pattern. In microglandular hyperplasia, cellular atypia is minimal and focal; furthermore, the glandular cells may have characteristic subnuclear vacuoles and intracytoplasmic mucin. In contrast, the clear cells in clear cell carcinoma contain glycogen, but do not contain intracytoplasmic mucin or subnuclear vacuoles.(2) Arias-Stellas change occur in endometrial and endocervical glands. Glands take on a tortuous profile and are lined by clear and hobnailed cells with cytologic atypia, thus can resemble clear cell carcinoma. However, the Arias-Stellas reaction is usually focal, affecting only a few glands. Furthermore, Arias-Stellas is generally associated with pregnancy and one may find accompanying decidual change in the cervical stroma.
A bimodal distribution exists with the major peak occurring in young women in their 20s. The second smaller peak occurs in elderly women in their 70s. Two-thirds of the women have a history of DES exposure in utero. Thus, it is important to note that cases do occur sporadically, as one-third of women do not have a history of DES exposure.
One text (Nucci) stated for patients with DES exposure, the neoplasm presented in the earlier age group, whereas sporadic cases occurred in the older age group.2 However, other texts (Rosai and Fletcher) do not make this assertion. Either way, there was agreement that the risk is low, even for women with DES exposure. Approximately 1 in 1000 exposed women develop clear cell adenocarcinoma.3,4 The risk is increased the earlier the exposure to DES (before 12th week of gestation).
Patients may be asymptomatic, or present with vaginal bleeding and dyspareunia. Sometimes, a palpable nodular or polypoid mass may be evident on exam.
Treatment involves radical hysterectomy with lymphadenectomy and concurrent chemoradiation. Total vaginectomy or even exenteration may be necessary depending on extent of the lesion.
Outcome is generally good with stage being the most important prognostic factor. 5 and 10 year survival rates are 91 and 85% respectively for stage 1 lesions while 5 year survival rates are 0% for stage 4 lesions.3 Metastases tends to occur in pelvic lymph nodes and lungs. Recurrence can occur up to 19 years after treatment of the primary tumor.1
→Like its counterpart in the vagina, clear cell adenocarcinoma of the cervix is associated with DES exposure in utero.
→Key differential diagnostic entities include microglandular hyperplasia and Arias-Stellas reaction.
→The most prevalent tumor cell type is hobnail cells, in which the nuclei protrude into the cystic lumens.
• Vagina : Clear Cell Adenocarcinoma
• Endometrium : Arias-Stella Reaction
• Cervix : Microglandular Adenosis (Hyperplasia)
1 Kurman RJ, Norris HJ, Wilkinson E. Tumors of the Cervix, Vagina and Vulva: Atlas of Tumor Pathology. Third Series Fascicle 4. Washington DC; AFIP: 1990: 89-90, 153-7.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 183-4.
3 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 720-1.
4 Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 1512-3.