
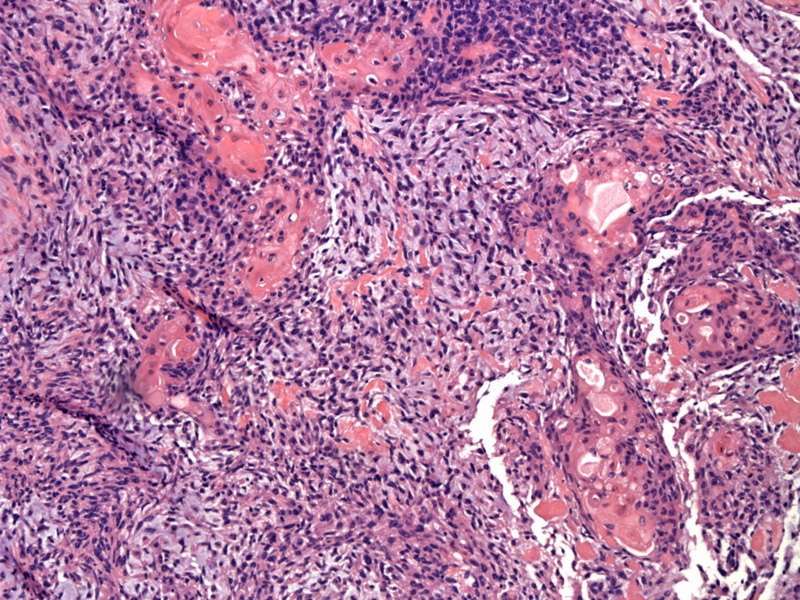
A proliferation of spindle cells is prominent. This particular tumor was designated as a spindle cell carcinoma, as it is comprised mainly of squamous and spindle cells. No giant cells were identified. The spindle cell stromal and epithelial components blend into each other.
Nests of neoplastic squamous cells (pink abundant cytoplasm) change inperceptibly into tapered spindle cells. The squamous component demonstrates fairly pleomorphic cytologic features with enlarged nuclei.
A closer view of the streaming fascicles of spindle cells is seen here.
The neoplastic immature mesenhymal cells are percolating through a myxoid (bluish) stroma on the right image. Note the respiratory epithelium on the upper left.
The epithelial component is often squamous, but poorly formed glands can also be present.
Sarcomatoid carcinoma, according to the current WHO definition, encompasses a group of NSCLCs which exhibit sarcomatous differentiation. Depending on their morphology and the bias of the pathologist, these tumors may be called pleomorphic carcinoma, spindle cell carcinoma, giant cell carcinoma, carcinosarcoma or pulmonary blastoma.
Spindle cell carcinomas (also known as spindle cell squamous cell carcinomas or confusingly, sarcomatoid carcinomas) are composed of spindle cells, but with an morphologically or immunohistochemically evident epithelial component. Giant cell carcinomas (extremely rare) have a prominent presence of tumor giant cells. If the carcinomatous and sarcomatous components are quite distinct, then carcinosarcoma is often used (Rosai).
These tumors are quite rare and account for only 1% of all lung cancers. They are more common in men than women with mean age of 60. The exception to this age range is pulmonary blastoma, which occurs in the 3rd and 4th decades.
Again, as with all lung cancers, symptoms depend on the location of the tumor. Central tumors cause post-obstructive pneumonia, cough and hemoptysis, while peripheral tumors may remain asymptomatic until they invade the pleura and chest wall (Zander).
Poor; comparable to other NSCLCs.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 185.
Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 397.
Zander DS, Farver CF. Pulmonary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2008: 558.