
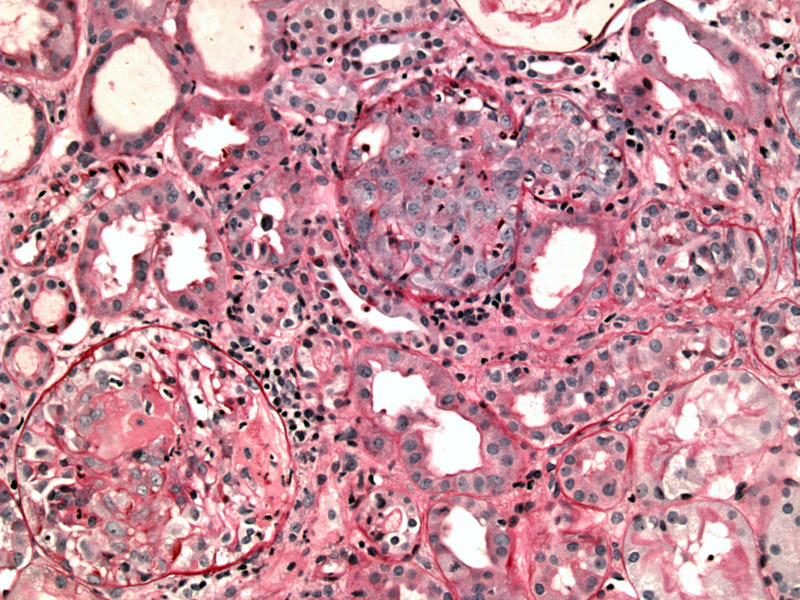
PAS stain highlights the basement membrane, outline tubules, vessels and glomeruli. The glomeruli on the bottom left image exhibits formation of a crescent. The more central glomerulus is cut such that mainly the cellular crescent is all that is seen.
Note the proliferation of parietal epithelial cells, protruding into Bowman's space.
A prominent almost circumferential cellular crescent can be appreciated. To the left there is tubular simplification.
Crescent formation is associated with fibrinoid necrosis as seen here (amorphous pink material) involving the upper portion of the glomerulus.
Trichrome better highlights the fibrinoid necrosis (seen as red) and collapse of the glomerular tuft.
Silver stain can highlight the breaks in the glomerular basement membrane.
Necrotizing arteritis of the arcuate is present, as seen here with fibrinoid necrosis of the vessel wall and inflammation (Zhou). Vasculitis is identified in only about 10-20% of biopsy specimens overall, however.
The interstitium is commonly very active with infiltrates consisting of monocytes, plasma cells and some neutrophils and eosinophils.
Crescentic glomerulonephritis, also known Rapidly Progressive Crescentic Glomerulonephritis (RPGN), describes a broad group of glomerulonephritides where the glomeruli are involved by epithelial crescents. Without treatment, RPGN is usually a severe and rapidly progressive disease. Clinical manifestations include hematuria, proteinuria that may reach nephrotic ranges, hypertension and edema (Kumar).
Rapidly progressive (crescentic) glomerulonephritis is classified by immune mechanism into three broad categories: Type I (anti-glomerular basement membrane disease); Type II (immune complex crescentic glomerulonephritis); and Type III (pauci-immune crescentic glomerulonephritis).
Type III RPGN or "pauci-immune glomerulonephritis" is so named because there is minimal or absent staining of immunoglobulins in the glomeruli on immunofluorescence (Rosai). However, I think this term can be a bit of a misnomer because it seems to suggest that these patients do not produce antibodies. But in fact, 90% of patients with pauci-immune glomerulonephritis elaborate antineutrophil cytoplasmic antibodies (ANCA) of either the cytoplasmic (C-ANCA) type or perinuclear (P-ANCA) type (Zhou).
Pauci-immune glomerulonephritis can be systemic such as in Wegener granulomatosis or microscopic polyarteritis or limited to the kidney. ANCA targeted twoard myeloperoxidase leads to perinuclear staining (p-ANCA) and is more often seen in microscopic polyangiitis and renal limited vasculitis, whereas ANCA targeted toward proteinase 3 causes cytoplasmic staining (c-ANCA) and is usually seen in Wegener granulomatosis.
Microscopically, the key histologic features include: (1) crescent formation which are proliferations of parietal epithelial cells as well as migration of monocytes and macrophages -- these crescents project into Bowman's space; (2) prominent fibrin strands between the cellular layers of the crescents; (3) ruptures in the glomerular basement membrane as demonstrated by silver stain; (4) over time, the glomerular tuft becomes compressed and may become completely sclerotic.
Usually affects the elderly (peak age at diagnosis is in the 6th and 7th decades). Pulmonary hemorrhage and acute renal failure are common presenting symptoms. Most (3/4) of patients also have a systemic vasculitis (ie. Wegener granulomatosis, microscopic polyangiitis)(Zhou).
High dose corticosteroids and immunosuppresive agents. Transplantation is appropriate for those with ESRD.
Initial remission may be obtained in up to 80% of patients, but disease recurrence is frequent, requiring maintenance therapy. With adequate support, the 5 year survival is on the order of 60-80%. Recurrence after transplantation affects about 20%.
• Lung : Microscopic Polyangiitis
• Lung : Wegener Granulomatosis
Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 977.
Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004: 1196-1200.
Zhou M, Magi-Galluzzi, C. Genitourinary Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elvesier; 2006: 381-384.