
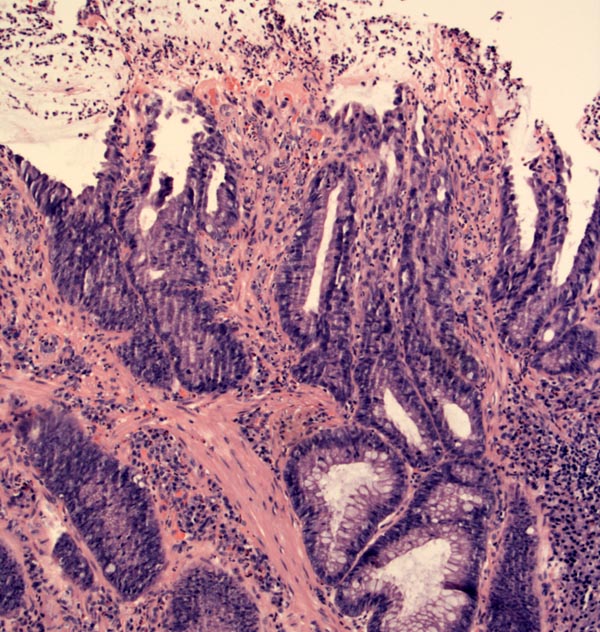
Inflammatory cloacogenic polyps show surface erosion with overlying fibrin and neutrophils. Irregular glandular shapes are evident, with focal cystic change.
The lamina propria is replaced by fibromuscular tissue and a lymphoplasmacytic infiltrate. Noting the growth of smooth muscle fibers between crypts and underneath crypt bases is key to diagnosing this entity. Underlying the erosion is granulation tissue harbouring red cells.
Another polyp along the anal verge, again showing surface injury and glandular distortion.
The expansion of the lamina propria due to granulation type tissue forms broad polypoid areas.
Note the hyperplasia of fibromuscular tissue and cystically dilated glands.
Inflammatory cloacogenic polyps, rectal prolapse, solitary rectal ulcer syndrome (SRUS), and colitis cystica profunda (CCP) are different manifestations of what is currently termed "mucosal prolapse syndrome". All these entities share a similar pathogenesis and thus, demonstrate similar histopathology. Furthermore, the co-occurrence of these conditions is common. For example, rectal prolapse affects 85-90% of patients with SRUS and 54% of patients with CCP. 3
The pathogenesis is thought to be peristalsis-induced and sheer injury (traction and torsion of the bowel mucosa) causing a small segment of mucosal prolapse. The repair mechanism involves replaces the lamina propria with fibromuscular tissue, which is THE KEY FEATURE common to all entities under this syndrome.2 The crypts may be elongated, branching, villiform and hyperplastic, simulating an adenomatous polyp. Furthermore, there may also be irregularly-shaped glands can be "trapped" by this fibromuscular stroma, scarily mimicking cancer. Focus on the fibromuscular hyperplasia of the lamina propria.
A few words about the other entities …
Rectal prolapse: Defined as a protrusion of some or all layers of the rectal wall. Complete prolapse involves the entire rectal wall and is essentially an intussusception. The prolapse may not necessarily be visible, even with straining. There is a bimodal age range (infancy and after age 40) and is more common in women. The lesions are those described in SRUS, PCP and inflammatory cloacogenic polyps.
Solitary rectal ulcer syndrome: Due to repeated straining, the shear stress on the rectal mucosa creates an erosion/ulceration. These lesions tend are located at the anterior anal canal 4-10 cm proximal to the anal verge.2 Note that SRUS is a misnomer because the ulcers may be multiple and ulceration is a late feature and may not always be present.3
Colitis cystica profunda: See our separate case for information on this entity.
Inflammatory cloacogenic polyp: Usually presents in an older population as a small polyp at the anorectal junction. The histological features are identical to those found in SRUS, with irregular, villiform crypts, smooth muscle proliferation in the lamina propria, surface erosion and possibly entrapped glands in the lamina propria (like colitis cystica profunda).
Mucosal prolapse syndromes (in general) occur in 3rd to 4th decades with a slight female predominance. 1,3 Presents with anorectal symptoms such as rectal bleeding, pain, diarrhea and difficulty defecating (e.g. straining, constipation, requiring digital disimpaction). Up to 50% may present with incontinence. 3 . A lesion (either an ulcer, induration, erythema and/or polypoid lesion) will be found in the anal mucosa.
Inflammatory cloacogenic polyp: Occurs at a later age at 5th to 7th decades with a slight female predominance. 1,3 A polypoid lesion is located at the anal verge (anorectal junction).
Stool softeners and increased dietary fiber. Surgery is considered for refractory cases.
Chronic relapsing disease
• Colon : Colitis Cystica Profunda
1 Iacobuzio-Donahue CA, Montgomery EA. Gastrointestinal and Liver Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier; 2005: 338-9, 398-400.
2 Odze RD, Goldblum JR, Crawford, JM. Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas. Philadelphia, PA: Elsevier; 2004: 240-1,331-3.
3 Fenoglio-Preiser CM, et al. Gastrointestinal Pathology: An Atlas and Text. 3rd Ed. Philadelphia, PA: Lippincoott Williams & Wilkins; 2008: 760-3,1060-1.