System: Skin: Epidermis: Malignant: Basal Cell Carcinoma


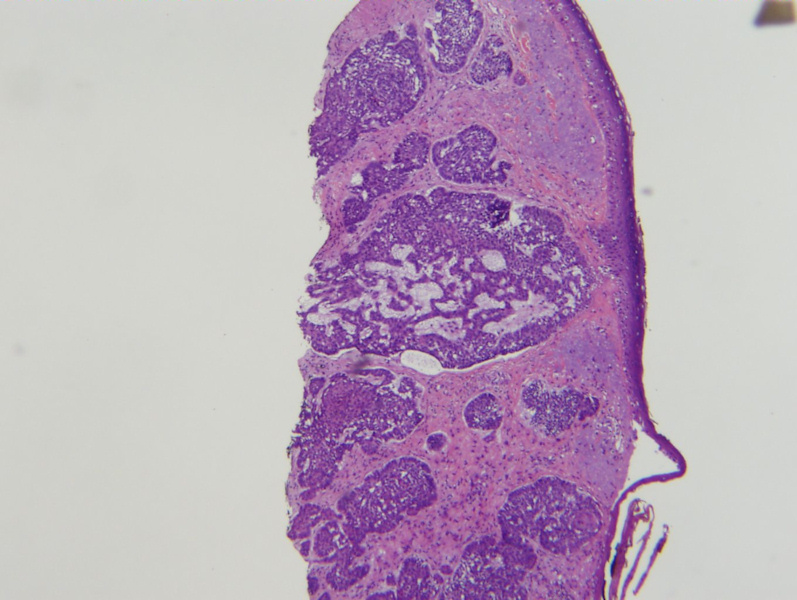
Case 1: Nodular or nodulocystic BCC. A cystic appearance due to necrosis of centrally located cells, adjacent to an accumulation of mucin occurs. In some cases, projections of the tumor cells produce a reticular formation.
In this high power view, one cell islets with the typical peripheral palisading and disorganized central region.
Case 2: In the superficial type, basaloid nests are attached to the epidermis and there are skip areas where the epidermis is normal.
Case 3: In the infiltrative subtype, tumor cells penetrate deeply among the underlying collagen fascicles. The cell nests are angulated and irregular.
Case 4: In the morpheaform or sclerosing pattern, the basaloid cells form angulated and irregular strands or nests similar to the infiltrative subtype, but the stroma demonstrates prominent fibrosis.
This chart depicts some of the proposed classification systems for BCC.
Basal cell carcinoma is now considered an adnexal tumor with follicular differentiation (Busam). It is considered the most common skin cancer and mainly occurs on sun-exposed skin.
Histologically, BCCs are characterized by basaloid cells that bud from the epidermis or follicles. There is prominent peripheral palisading of the basaloid cells, myxoid stroma and artifactual retraction/clefting (Busam). Other common features include solar elastosis in the dermis, mitotic figures, apoptotic bodies, amyloid deposition, calcifications and an inflammatory infiltrate composed of lymphocytes and plasma cells (Busam, Rapini).
Patterns of BCC are important to recognized as they are indicators of biologic behavior. BCCs are traditionally classified as "undifferentiated" (solid growth) versus "differentiated", demonstrating differentiation toward specific cell lines (e.g. eccrine, sebaceous).
Undifferentiated BCCs: It is easiest to think of patterns as indolent or aggressive growth patterns. The indolent growth patterns are superficial and nodular types. The aggressive growth patterns are infiltrative, morpheiform/sclerosing and metatypical types (Crowson).
Differentiated BCCs: These BCCs show differentiation toward certain cell lines, and it is important to recognize them as to correctly identify them as BCC, however, the various subtypes do not change the prognosis. Included in this category are keratotic BCC, adenoid cystic BCC, pigmented BCC, infundibulocystic BCC, follicular BCC, clear cell BCC, pleomorphic BCC, BCC with sweat duct differentiation, BCC with sebaceous differentiation and fibroepithelioma of Pinkus. This is not an exhaustive list, but I am exhausted just thinking about it.
Briefly, superficial BCCs are characterized by epithelial aggregates of basaloid cells that are still attached to the epidermis. These aggregates are multifocal and areas of normal epidermis (skip areas) are in between the proliferative nests (Busam).
Nodular BCC is likely the most common form of BCC, and is characterized by nodules of basaloid cells that bud or drop off from the epidermis. When cystic spaces from in the nodules, one may refer to the pattern as nodular/nodulocystic.
Micronodular BCC is similar to nodular BCC, however, the nests are smaller and clinically appears as a plaque with poorly demarcated borders. It may penetrate more deeply into the dermis or subcutis and has a higher rate of local recurrence. Thus, micronodular BCC is considered to be in between the nodular and aggressive subtypes in terms of behavior (Crowson).
Morpheaform BCC and infiltrative BCCs are characterized by irregularly-shaped and angulated aggregates of basaloid cells in strands and small nests. Single cells are not uncommon. These aggressive subtypes to penetrate deeply into the dermis and subcutis; perineural invasion is a risk. Note that morpheaform BCC is synonymous with sclerosing BCC and are associated with prominent stromal fibrosis. However, infiltrative BCC may not necessarily be morpheaform or sclerosing (Busam).
Metatypical BCC is considered to be synonymous with basosquamous BCC, and is an aggressive subtype. Areas of squamous differentiation (keratinization, intercellular bridging) are admixed with clear-cut BCCs. It may be difficult to distinguish between a squamous cell carcinoma and a basosquamous BCC in a small biopsy. Furthermore, mixed basal cell-squamous cell carcinomas (collision tumor) may also be a consideration (Crowson).
Usually arises on sun-exposed skin of adults, especially in fair-skinned individuals. UV light is the most important risk factor, followed by radiation, arsenice, coal tar derivatives and immunosuppression. Patients with xeroderma pigmentosuem (autosomal recessive disorder in which DNA damage caused by UV light cannot be repaired) and basal cell nevus syndrome/Gorlin syndrome (autosomal dominant disorder in which the PTCH gene is mutated) develop multiple BCCs, among other findings. Of interest, mutations of the PTCH gene have also been identified in sporadic BCCs (Busam).
The clinical appearance of a BCC depends on the histologic subtype. Classically, BCCs are described as a pearly red papule or nodule with a rolled up edge. This corresponds with a nodular pattern histologically. The superficial subtype appears as reddish plaques with variegated pigmentation and may be multifocal. Aggressive growth subtypes (e.g. infiltrative, morpheaform) appear as scaly, ill-defined, irregular plaques that may be elevated or depressed (Crowson).
Usually, BCC is only destructive locally and in exceptionally rare cases, may metastasize to lymph nodes, lungs and bones.
• Epidermis : Basal Cell Carcinoma, Infiltrating Type
• Epidermis : Basal Cell Carcinoma, Micronodular Type
• Epidermis : Basal Cell Carcinoma, Nodular Type
• Epidermis : Basal Cell Carcinoma, Superficial Type
• Epidermis : Basal cell carcinoma, Fibroepithelioma of Pinkus
• Epidermis : Basal Cell Carcinoma, Metatypical Type
Busam KJ. Dermatopathology: Foundations in Diagnostic Pathology 1st Ed. Philadelphia, PA: Elsevier; 2010: 389-397.
Crowson AN. Basal cell carcinoma: biology, morphology and clinical implications. Modern Pathology (2006) 19, S127-S147.
Rapini RP.Practical Dermatopathology. Philadelphia, PA: Elsevier; 2005: 249-252.